
Medical Journal
Published by
Faculty of Medical Sciences,
University of Sri Jayewardenepura,
Nugegoda,
Sri Lanka.
Original Articles
Knowledge, Attitude and Practice of Self- Medication and its associated factors among Medical and nursing undergraduates in a selected University in Sri Lanka
Subramaniyam M1*, Senanayake S C1, Manjika M S2, Wickremasinghe R3
1Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka
2Department of Community Medicine, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka
3Department of Parasitology, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka
*mayoomayoori007@gmail.com
Abstract
Background: Self-medication is a widespread practise globally and is characterised as a patient using medication on their own without seeking advice from a healthcare professional. It is a crucial aspect of how patients behave when dealing with disease, particularly when they believe they don’t need to see a doctor for common health issues. Although self- medication practice can save time and reduce treatment costs, it can also be harmful.
Objective: To describe the knowledge, attitude and self- practice among medical and nursing undergraduates in a selected University in Sri Lanka.
Method: A descriptive-cross sectional study was conducted among medical and nursing undergraduates of the faculty of Medical Sciences, University of Sri Jayewardenepura, using a self – administered Google form.
Results: A total of 442 students were included in this study; 77 of them were nursing undergraduates and 365 were medical undergraduates. 87.8% were in the age group of 21-25 years. There was a preponderance of females (71.0%). Within last six months, 40.5% of them self medicated more than twice and only 34.4% consulted the doctor when they fell sick. The common conditions treated by self- medication are pain (86%) followed by cold and cough (70.8%) and fever (64.3%). Most of the respondents got their information from family and friends (64.9%). Majority of respondents declared that community pharmacy (57.2%) was the main source for obtaining the medication. 205 (46.4%) of the respondents had good knowledge and 186 (42.1%) had good attitude regarding self- medication.
Conclusion: The information gathered by this study, although only among undergraduate students, can help create specific programs and policies to encourage responsible self-medication and improve healthcare results. Additionally, more research may be needed to understand the cultural and contextual factors that affect these patterns.
Introduction
Self-medication is a widespread practise globally and is characterised as a patient using medication on his own without seeking advice from a healthcare professional. It is a crucial aspect of how patients behave when dealing with disease, particularly when they believe they don’t need to see a doctor for common health issues. Although self- medication practice can save time and reduce treatment costs, it can also be harmful. However, the WHO has emphasised the importance of appropriate self-medication for the prevention and treatment of common illnesses (Goel, 2013). However, this responsible self-medication is limited to over the counter (OTC) medications, for self-identifiable conditions, and at the same time, only if the user is aware of the medication’s possible side effects, drug interactions, and when to consult a doctor. A certain amount of understanding is necessary to practise safe self-medication; otherwise, it may result in incorrect or delayed diagnosis, increased pathogen resistance, and higher morbidity due to adverse effects and drug interactions, such as drug-alcohol (Goel, 2013).
Studies showed that, particularly among young people, self-medication tendencies are on the rise. This can be attributed to socioeconomic factors like lifestyle, easy access to medications, increased ability to treat some illnesses on one’s own, availability of pharmaceuticals, sociodemographic and epidemiological data, accessibility of healthcare and medical professionals, exposure to advertising in society and law, high levels of education, and professional status. Self-medication is not entirely forbidden, but the WHO has established standards for responsible self-medication. Therefore, it is important to understand how often self-medication is among medical undergraduate students (Lokeesan & Laavanya, 2019).
In Sri Lanka, very few studies have been carried out regarding this topic. Therefore, this study was done to obtain insight into self-medication and to describe the knowledge, attitude, self-practice and factors associated with self-medication among nursing and medical undergraduates in a selected university in Sri Lanka.
Methodology
A descriptive cross-sectional study was done in the Faculty of Medical Sciences, University of Sri Jayewardenepura. Sample size calculation was computed using the Lwanga and Lemeshow (1991) formula. The total sample constituted of 442 participants. Among them, 77 were nursing undergraduates and 365 were medical undergraduates (1st year = 97, 2nd year = 74, 3rd year =56, 4th year = 69, 5th year = 69). Participants were recruited using a convenient sampling method.
Data were collected using a by a self- administered Google form which was formulated in English. The questionnaire had 3 sections: information regarding sociodemographic factors, knowledge on self-medication, and attitude and practice of self-medication.
Data were analyzed using SPSS software version 16 Quantitative data were described using frequency distribution and mean values. Qualitative data were presented using percentages. Associations were assessed using the Chi-squared test. Statistical significance was taken as p<0.05.
Ethical approval for this study was obtained from the Ethics Review Committee of the Faculty of Medical Sciences, University of Sri Jayewardenepura.
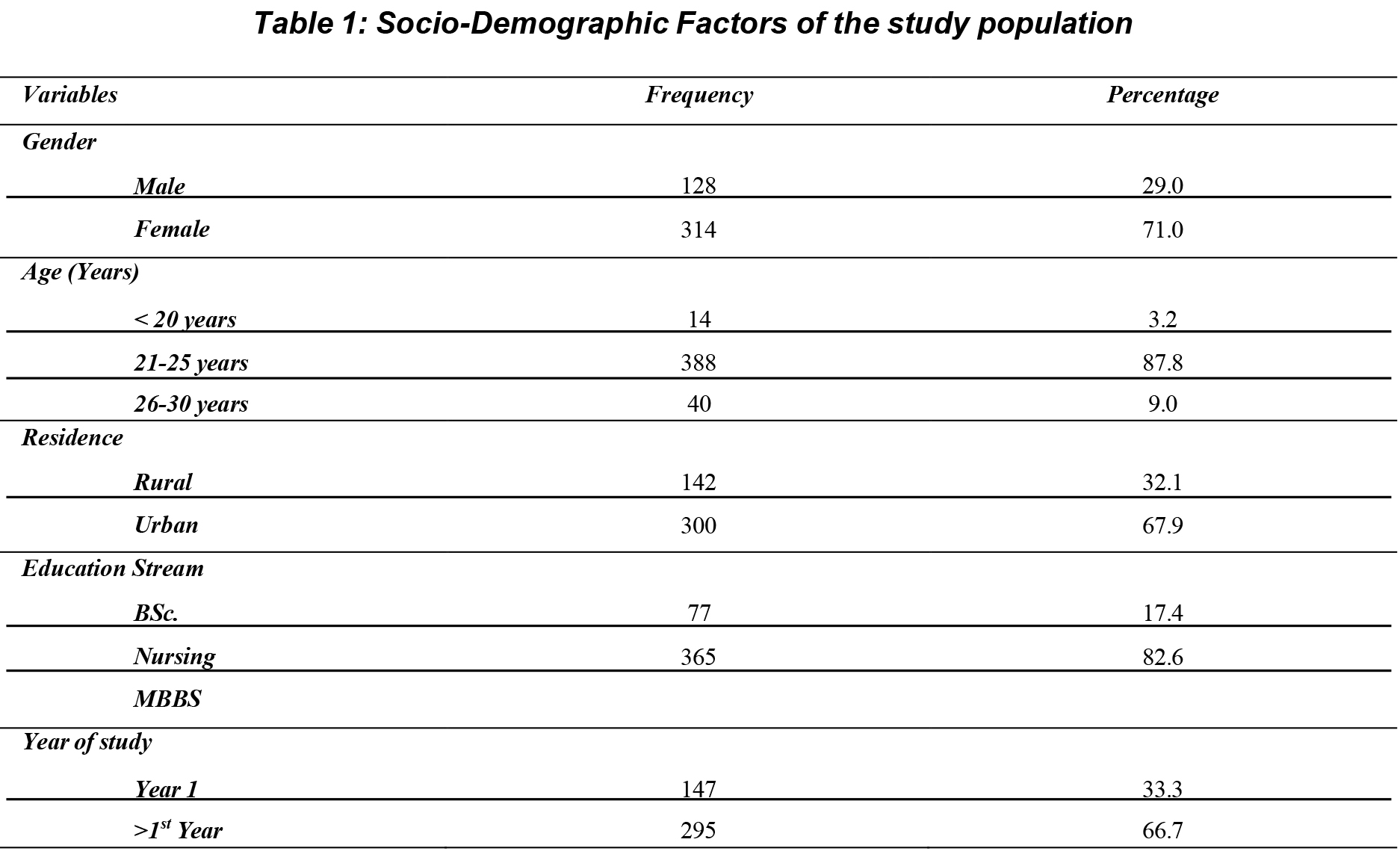
Table 1 shows that out of 442 respondents 388, (87.8%) were in age group of 21-25 years, 40 (9%) were in age group of 26-30 years and 14 (3.2%) were in age group of less than 20 years. 314(71%) were female and 128(29%) were male, and 300 (67.9%) were form urban area and the rest from rural area. With regard to stream of education, 365(82.6%) were medical students and 77(17.4%) were nursing undergraduates. 66.7% were above the 1st year
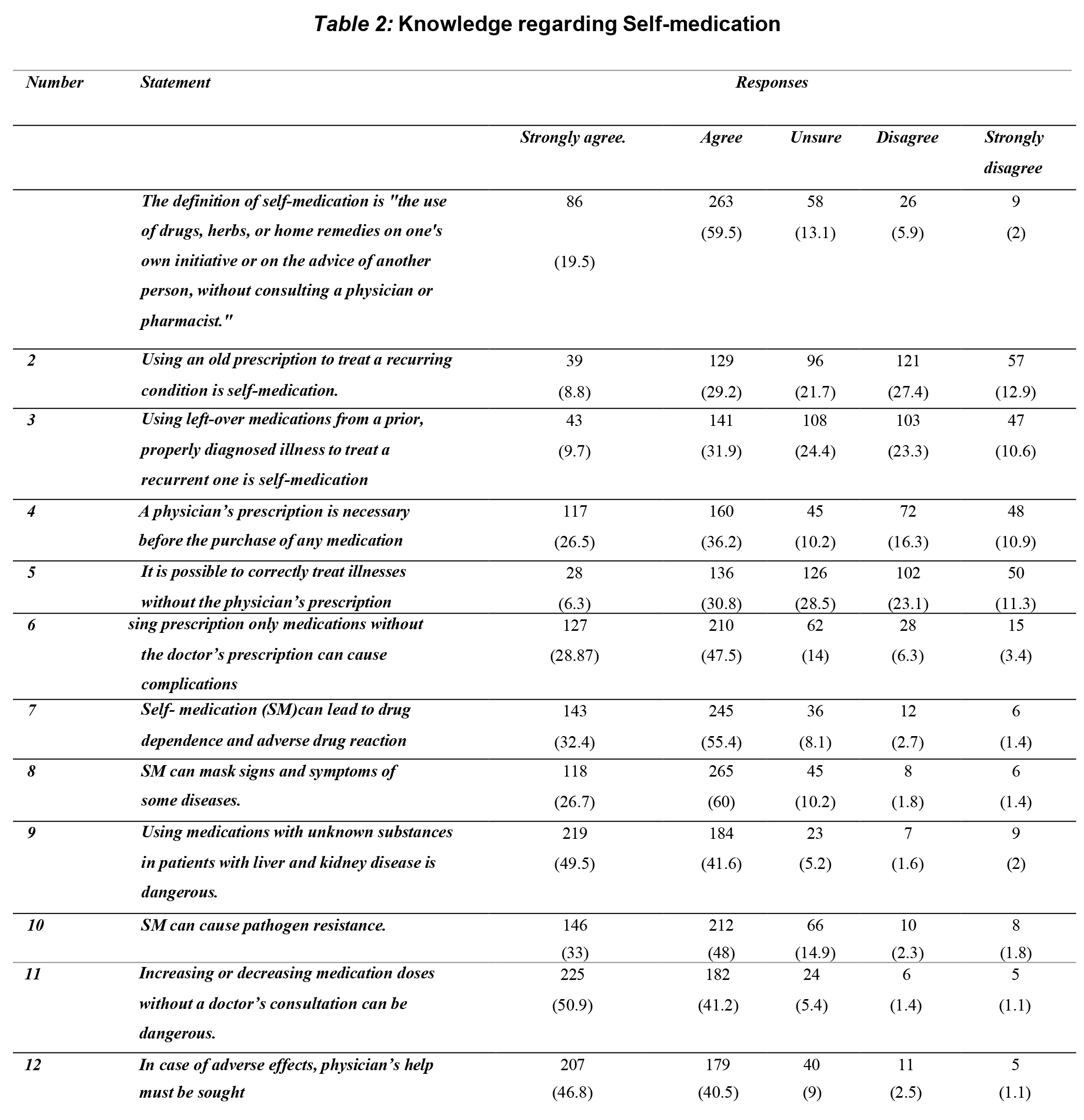
Respondents’ level of knowledge regarding self-medication
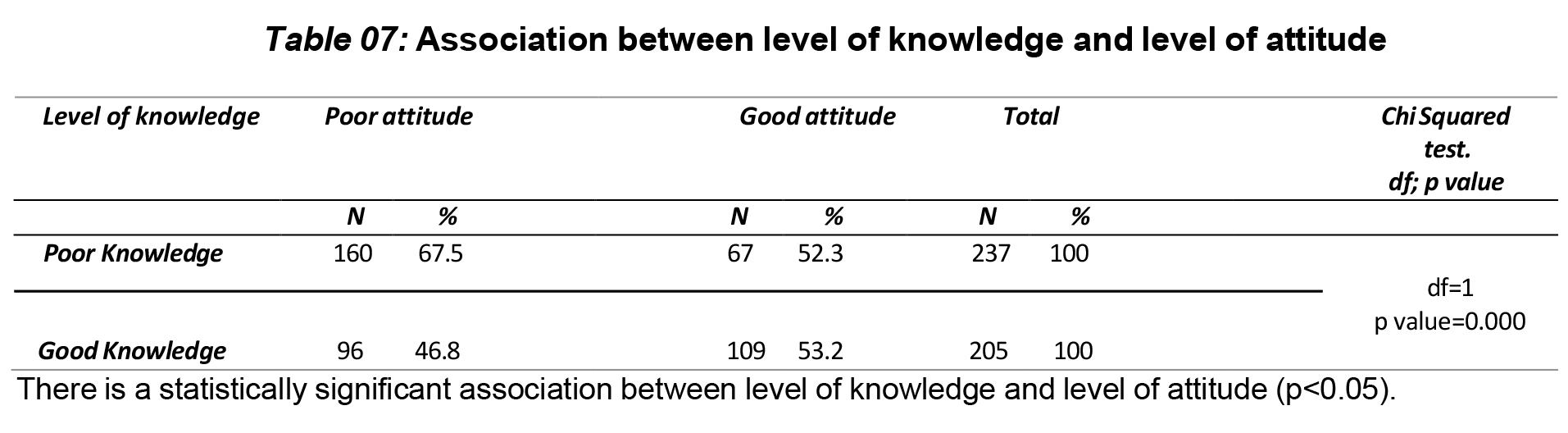
This study shows that237(53.6%) respondents had poor level of knowledge regarding self-medication, followed by 205(46.4%) respondents had good level of knowledge regarding self-medication.
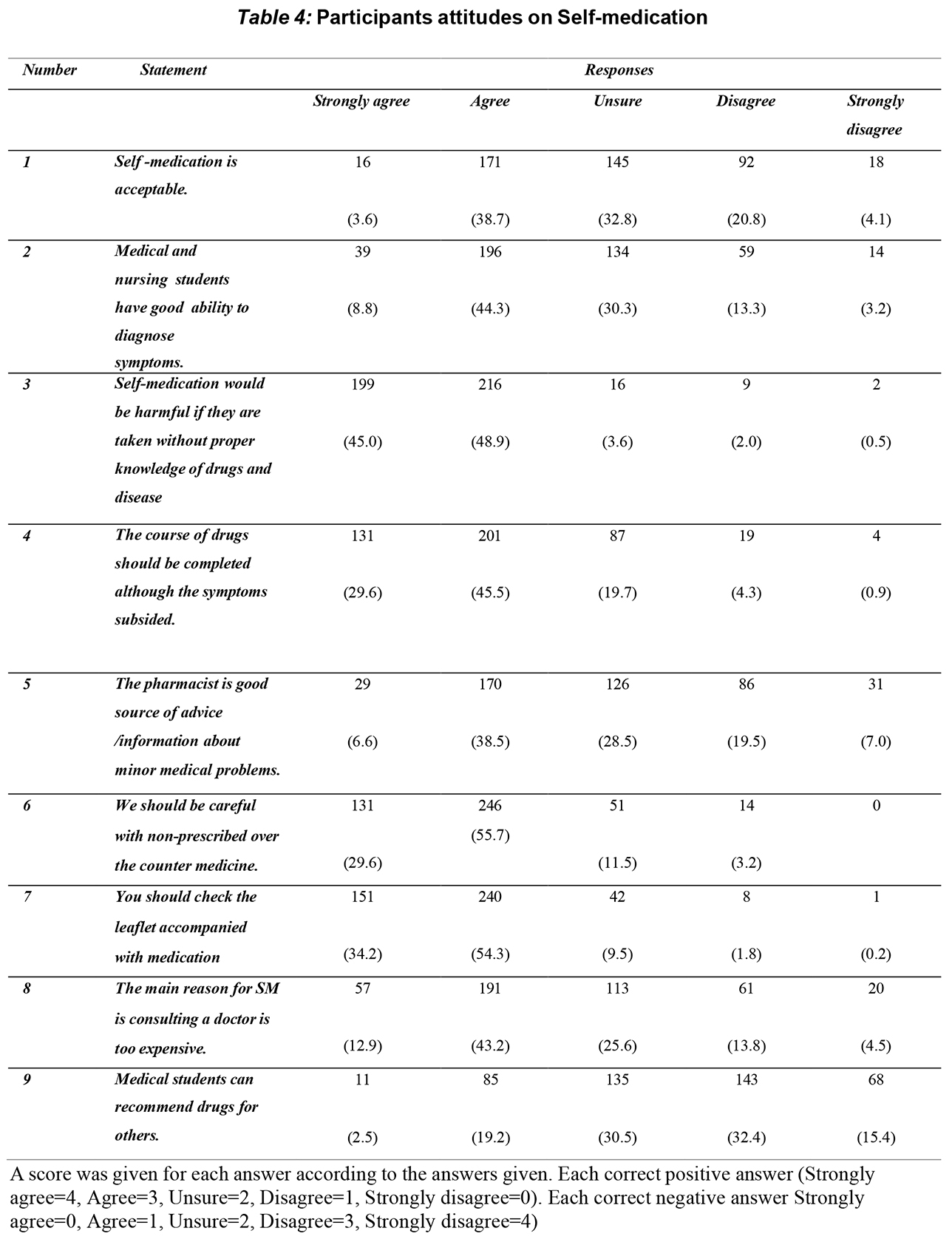
Respondents’ level of attitude regarding self-medication
This study shows that 256 (57.9%) respondents had poor attitude regarding self- medication, and 186 (42.1%) respondents had a good attitude regarding self-medication. When considering self-practice among the among our study population, the majority, 153 (34.6%) practice self-medication when they fall sick, followed by consulting a doctor 152 (34.6%). A minority of them ask suggestions from others, 62 (14%) and wait until symptoms subside, 75 (17%). When considering the prevalence of students taking self-medication, we observed that 40.5% of the students had taken self- medication more than twice in the last six months, 27.6% had taken it twice, 20.4% had taken it once and 11.5% had never taken self-medication in last six months.
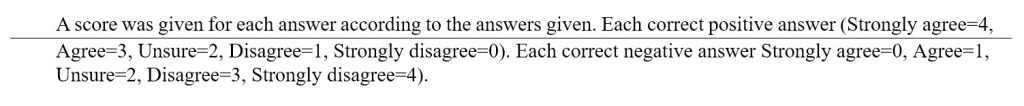
Among the reasons given for self- medication, a majority of respondents 292 (66.1%), felt that they had minor illness followed by prior experience, 201 (45.5 %). Participants claimed that common conditions treated by self-medication are pain (head ache, body ache and toothache), 380 (86%), cough and cold, 313 (70.8%) and fever 284 (64.3%). The following drugs were used by participants for self-medication: antacids 224 (50.7%), antibiotics 206 (46.6%), analgesics and antipyretics 202 (45.7%). Minority of them are using antihistamine 140 (31.7%), laxatives 26 (5.9%), antidepressants 6 (1.4%) n for SM.
According to NMRA guidelines, out of the drugs we listed, Paracetamol is the only drug which can be taken over the counter, but among our study population, 78% believes that Chlorphenamine is also an over-the-counter drug followed by Omeprazole (64.7) and Domperidone (60.3%). Minority of them believes that ibuprofen (20.6%), Fexofenadine (24.1%), Loratidine (33.7%), Antibiotics (46.1%), Alprazolam (4.8%) are also over the counter drugs.
With regard to the sources of self- medication, 253 (57.2%) of participants use community pharmacy as a source of self – medication. Participants receive information regarding drug dosage regimen through family and friends, 287 (64.9%), patient information leaflet 256 (57.9%), Textbooks 189 (42.8%), social media 118 (26.7%), and classroom 106 (24.0%).
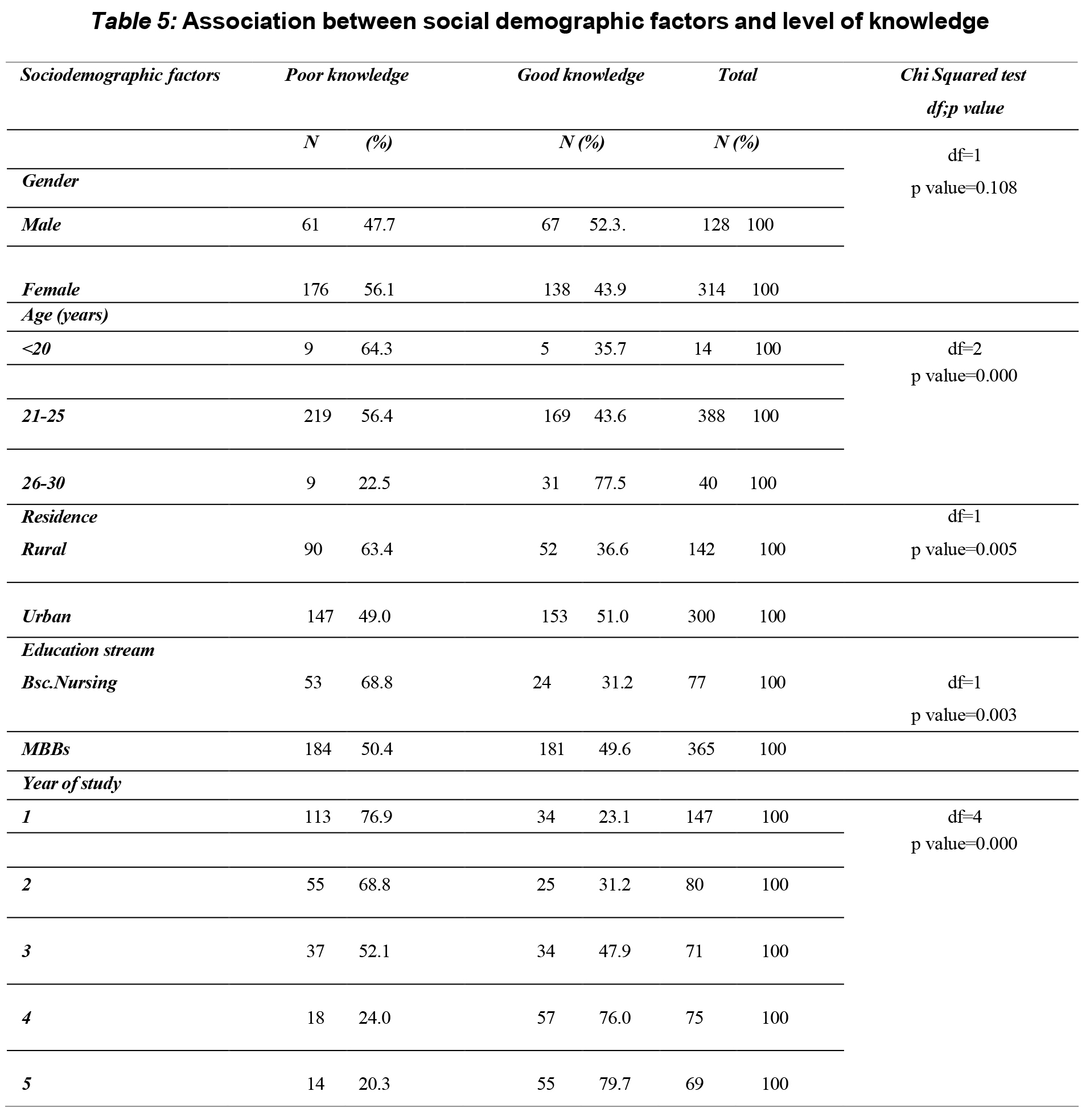
There was a statistically significant association between level of knowledge and age, residence, education stream and year of study (p<0.05) but there is no statistically significant association between level of knowledge and gender (p>0.05)
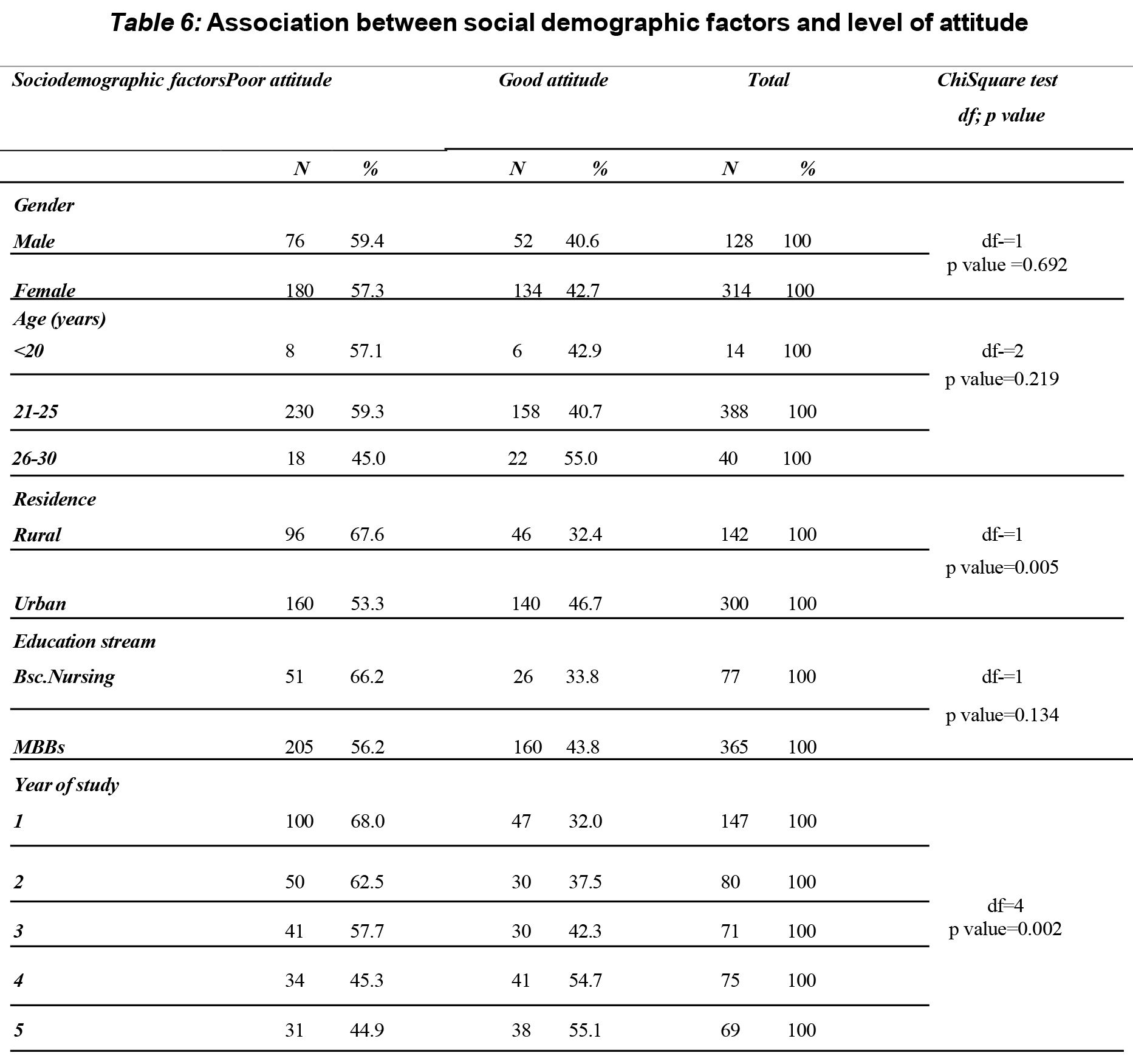
There is a statistically significant association between level of attitude with residence and year of study (p<0.05). There is no significant association between level of attitude with gender, age and education stream.
Discussion
Considering the level of knowledge regarding self-medicatio, 46.4% respondent had good knowledge, whereas 53.6% had poor knowledge. In contrast to this, study done in Nepal among medical students showed that majority of the participants had good knowledge (Mehta & Sharma, 2015) .Our study reveals a significant disparity in self-medication knowledge levels between medical and nursing students within the university. Specifically, 49.6% of medical students exhibit good knowledge, while only 31.2% of nursing students attain a similar level of understanding. This marked contrast can be attributed to curriculum disparities and varied clinical exposures between the two groups. Medical students tend to benefit from comprehensive pharmacology coursework, enabling them to acquire knowledge about drug side effects, advantages, and disadvantages. The differences in understanding highlight the need for tailored educational initiatives for nursing students. These programs should focus on improving their knowledge of self-medication and its risks. Significantly, an upward trend in knowledge emerges among medical students with each successive year of study, particularly in the fourth and fifth years, presumably due to heightened clinical re and advanced pharmacology exposure.
In contrast to the study conducted in Bahrain, which reported a favorable attitude towards self-medication among the majority of medical students (76.9%), only 42.1% of the respondents in this current study evince a positive attitude (James et al., 2006).. This divergence may be attributed to divergent cultural norms, healthcare practices, or the distinctive environment within this university. This divergence may be attributed to divergent cultural norms, healthcare practices, or the distinctive environment within this university.
The study sheds light on substantial self- medication practices, with a noteworthy 86% of respondents resorting to self-administered medication for pain, 70.8% for cough and cold, and 64.3% for fever. These findings mirror those of prior research conducted in India which documented analogous trends of self-medication for common ailments. It is pivotal to underline that self-medication patterns for pain, cough, and cold, and fever might be indicative of the accessibility and perceived efficacy of over-the-counter medications for these symptomatic presentations (Pandya et al., 2013).
The research underscores that commonly self-administered drugs encompass antacids (50.7%), antibiotics (46.6%), analgesics (45.7%), and antipyretics (45.7%). In the study done in Nepal, majority used antipyretics (46.8%), antibiotics (40.3%), and anti-allergies (35.5%). In our study, it is noteworthy that antibiotic usage is relatively high at 46.6% (Mehta & Sharma, 2015), a finding that should evoke concern owing to its implications for antibiotic resistance and potential adverse effects. Certainly, this emphasizes the need for campaigns that educate and raise awareness about using antibiotics responsibly. It’s crucial to help reduce these potential risks effectively.
The primary motivations for self-medication divulged in the study are minor illnesses (66.1%) and prior experience with specific diseases (45.5%). This finding is in congruence with the findings of the study conducted in Nepal among medical students, major reason was minor illness (79.4%), and the diseases of prior experience (61.9%) (Mehta & Sharma, 2015). Certainly, individuals often attempt to self- treat minor health issues. Nevertheless, these seemingly insignificant ailments may occasionally conceal underlying, more complex conditions. Therefore, it becomes crucial to impart public health education to dispel this misconception and emphasize the importance of seeking professional medical evaluation when needed.
The data delineates that family and friends serve as the most prominent sources of information on drug dosage regimens (64.9%), closely followed by patient information leaflets (57.9%). %). In the study done in Nigeria, patient information leaflets (32.3%) and family and friends (22.1%) were the most common sources of information (Akande- Sholabi et al., 2021). This underscores the substantial role that social networks and patient information materials play in shaping self-medication practices. Vigilant efforts to ensure the dissemination of accurate and reliable information through these channels can substantively contribute to safer self- medication practices.
Majority of students receive self-medication drugs from Community pharmacy 57.2% and Friends/ Family 55.2%. This finding is in congruence with the findings of the study conducted in Ethiopia among Undergraduate Health Science Students, where majority received self-medication drugs from Pharmacy (79.5%) and relatives (14.1%) (Siraj et al., 2022).
It’s important to educate students about the right way to use these medicines and to seek professional help when needed. Also, better rules for selling these medications might be necessary to ensure safe use by students.
In conclusion, this study provides valuable information about knowledge, attitudes, and practices of self-medication among medical and nursing students in Sri Lanka. This information can help create specific programs and policies to encourage responsible self-medication and improve healthcare results. Additionally, more research may be needed to understand the cultural and contextual factors that affect these patterns
Conclusions
In conclusion, this study provides valuable information about knowledge, attitudes, and practices of self-medication among medical and nursing students in Sri Lanka. This information can help create specific programs and policies to encourage responsible self-medication and improve healthcare results. Additionally, more research may be needed to understand the cultural and contextual factors that affect these patterns. This study was conducted only among medical and nursing students and the results cannot be generalized. 205 (46.4%) of the respondents had good knowledge and 186 (42.1%) had good attitude regarding self- medication.
Recommendations
This study was only conducted in one University . The study will be useful in providing baseline data about self-medication prevalence and practise. Conducting counselling programmes on the potential dangers of self-medication can aid in preventing the negative effects of unauthorised medication in Sri Lanka. Large-scale studies of the same kind can be carried out in several contexts. By highlighting the risks associated with self- medication, self-medication can also be covered in classes. Monitoring systems amongst the important stake holders can be used to establish restrictions on the sale of pharmaceuticals with potentially dangerous consequences. Actions can also be done to prevent chemists from selling over-the-counter medications. Only pharmacy graduates should be permitted to sell the medications.
Acknowledgment
The authors would like to thank the medical and nursing students for their participation.
References
- Akande-Sholabi, , Ajamu, A. T., & Adisa, R. (2021). Prevalence, knowledge and perception of self-medication practice among undergraduate healthcare students. Journal of Pharmaceutical Policy and Practice, 14(1).
- Alduraibi, K., & Altowayan, W. M. (2022). A cross-sectional survey: knowledge, attitudes, and practices of self-medication in medical and pharmacy students. BMC Health Services Research, 22(1).
- Goel, D. D. (2013). Self-medication patterns among nursing students in North India. IOSR Journal of Dental and Medical Sciences, 11(4), 14–17.
- James, , Handu, S. S., Al Khaja, K. A. J., Otoom, S., & Sequeira, R. P. (2006). Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Medical Principles and Practice, 15(4), 270–275.
- Lokeesan, , & Laavanya, L. (2019). Self- Medication Practices among Undergraduate Nursing Students. International Journal of Pharma Research and Health Sciences, 7(1), 2894–2898.
- Lv, , Zhou, Z., Xu, G., Yang, D., Wu, L., Shen, Q., Jiang, M., Wang, X., Zhao, G., Yang, S., & Fang, Y. (2014). Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Tropical Medicine & International Health : TM & IH, 19(7), 769– 779.
- Mehta, R. K., & Sharma, S. (2015). Knowledge, Attitude and Practice of Self- Medication among Medical 4(1), 89–96.
- Pandya, R., Jhaveri, , Vyas, F., & Patel, V. (2013). Prevalence, pattern and perceptions of self-medication in medical students. International Journal of Basic & ClinicalPharmacology, 2(3), 1.
- Siraj, E. A., Yayehrad, A. T., Kassaw, A. T., Kassahun, D., Solomon, E., Abdela, H., Gizachew, G., & Awoke, E. (2022). Self- Medication Prevalence and Factors Associated with Knowledge and Attitude Towards Self- Medication Among Undergraduate Health Science Students at GAMBY Medical and Business College, Bahir Dar, Patient Preference and Adherence, 16, 3157–3172.
- Subashini, N., & Udayanga, L. (2020). Demographic, socio-economic and other associated risk factors for self-medication behaviour among university students of Sri Lanka: A cross sectional BMC Public Health, 20(1).
