Medical Journal
Published by
Faculty of Medical Sciences,
University of Sri Jayewardenepura,
Nugegoda,
Sri Lanka.
Perspective
Peer-assisted learning: a perspective of an Asian Medical School
Indrakumar J1, Matthias A T1*, Yogendranathan N1, Piyarathna C1, Kaluarachchi TR1, Gunatilake S B1, Navaretnam S1
1Department of Medicine, Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka
*thushara.matthias@gmail.com
Abstract
Background: Peer-assisted learning (PAL) has been practised informally in Sri Lankan medical schools for several years. This study explored the current practice, the students’ perceptions and drawbacks of PAL.
Methods: A descriptive cross-sectional study was conducted among 115 final-year students and 38 immediate graduates of the Faculty of Medical Sciences, University of Sri Jayewardenepura, Sri Lanka.
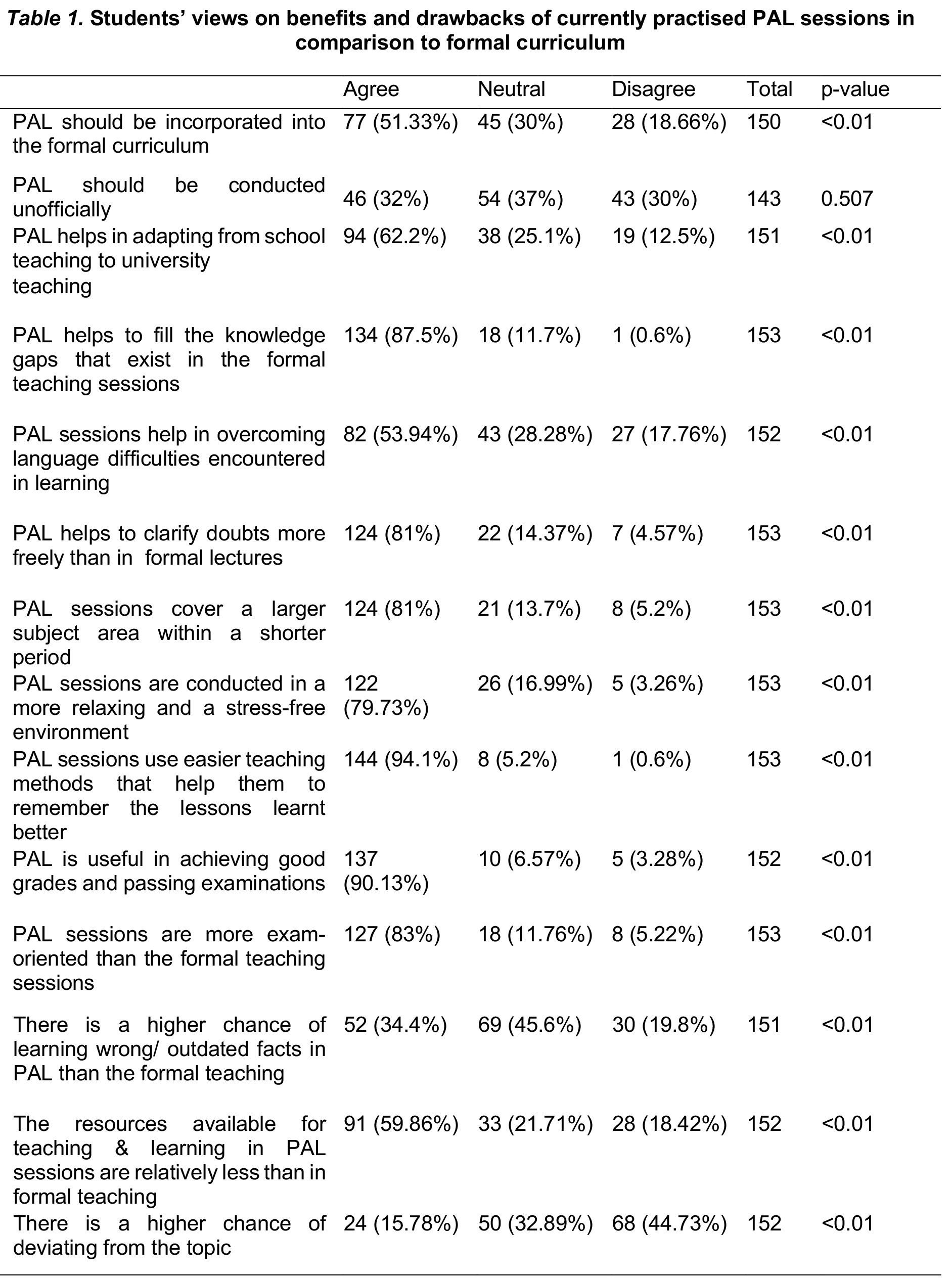
Results: The PAL sessions exhibited high popularity, particularly in the first two years (98.7%). The most preferred teaching sessions were Multiple Choice Questions (94.2%), Structured Essay Questions (93.9%), clinical case teaching (93.6%), and lectures (91.4%). A significant majority of students (90.13%) perceived PAL sessions as effective for exam success. Key reasons supporting PAL sessions included their ease (94.1%), bridging knowledge gaps (87.5%), providing a platform for addressing doubts freely (81%), and being exam-oriented (83%) (p<0.01). A majority (51.33%) expressed a desire for PAL sessions to be formally integrated into the curriculum (p<0.01). The primary drawback identified was the inadequacy of resources for teaching and learning (59.86%).
Conclusion: The results suggest that PAL is an effective and widely accepted teaching method in our medical school and most students feel that it should be incorporated into the formal curriculum as a supplementary teaching process.
Keywords: Cross-Sectional Studies, Schools, Medical, Sri Lanka, Curriculum, Students, Faculty
Introduction
Peer-assisted learning (PAL) is based on the key principle that peers help each other to learn, consolidate and improve their knowledge [1], [2]. It is a process whereby there is the acquisition of knowledge and skills through active help and support by peers[3] In the ever-evolving landscape of education, peer assisted learning has garnered significant attention for its potential to enhance the learning experience beyond traditional instructional methods.
Teaching is an integral part of a doctor-patient relationship. Engaging in such training would help them to develop their communication skills better. Further, exposing the medical students for teaching early in their career, will give them a better understanding and experience of the principles of teaching and learning which will enable them to become lifelong learners. As medical educators strive to prepare competent and compassionate physicians, understanding how peer interactions contribute to the holistic growth of medical students becomes essential.
PAL is being practised in some medical schools as a part of the formal curriculum. In the UK there is a formal student-led PAL scheme to teach clinical skills to third, fourth and fifth-year students [4] Certain medical schools offer senior medical students, the opportunity to teach junior medical students where fourth-year students participate in the teaching of first and second years in small group discussions and laboratory exercises [5] Peer-assisted learning is a vital aspect of active learning in medical education, enhancing knowledge retention and metacognitive awareness. In a peer-supported environment, students feel less apprehensive about making mistakes compared to interactions with faculty. This fosters collaborative problem-solving, providing numerous opportunities for students to identify and correct errors before examinations, and facilitating the effective development of clinical skills through continuous practice.[6]
In Sri Lankan medical schools, PAL is not a component of the formal medical curriculum. However, it is well-known that PAL has existed for many years in several medical faculties as an informal learning process. This process is organised by groups of successful students and is conducted in an informal manner parallel to the formal teaching. Although the faculty teachers were aware of this teaching process, they neither facilitated nor discouraged this. Participation in these classes is entirely voluntary.
In the Faculty of Medical Sciences, University of Sri Jayewardenepura too, PAL sessions have been conducted mainly aimed at the first two years. The so-called difficult topics have been discussed in these classes. Teaching methods consist principally of lectures and small group teaching sessions. These classes are usually conducted closer to the examinations. Repeat exam campaigns are also conducted for the unsuccessful students, mainly by the students who had succeeded at the first attempt both from the same year and senior batches. The graduates who had passed the most recent final MBBS examinations and were appointed as demonstrators in various departments of the faculty conduct informal theory, clinical classes, exam-oriented questions and answer sessions for students. There has been only one published Sri Lankan qualitative study exploring students’ experiences with PAL classes[7]. The study concluded that this student-initiated PAL process appears to be succeeding for the students. Their experiences may help implement a PAL process or even improve the formal teaching processes by incorporating PAL into the curriculum.
The purpose of our study is to explore the current practice of PAL, the perceptions of the final year medical students and immediate graduates in the Faculty of Medical Sciences, University of Sri Jayewardenepura, on the effectiveness of PAL and the drawbacks of PAL.
Methods
The Descriptive cross-sectional study was conducted among all the medical students who were in their final year in 2013 & those who had completed their Final MBBS in the year 2012 and Working temporarily as a demonstrator in the Faculty of Medical Sciences, University of Sri Jayewardenepura. Data were collected by a self-administered questionnaire and analysed using SPSS 17.0 software. A pretest was carried out to identify the pitfalls in the questionnaire. A total of 153 questionnaires were analysed, out of which 115 were final-year students and 38 were demonstrators.
The questionnaire was distributed voluntarily after obtaining informed consent from the participants. No personal details were obtained. Our study did not include any interventions on participants. Hence after discussing with the ethical approval committee of the Faculty of Medical Sciences, University of Sri Jayewardenepura no ethical issues were identified related to our stud.
The statistical analysis including demographical analysis was conducted using Microsoft Excel 2013, R software (version 4.0.3), and R-Studio (version 1.4.1106). Graphical analysis was also carried out using Excel 2013 and the proportions of the response rates concerning each factor were assessed under separate sections according to the questionnaire.
Results
Current practice of PAL:
Almost all students (99.3%) had participated in the PAL process either as learners or tutors at some stage of their medical career. Participation only as a learner, only as a tutor and as both learner & tutor were 49.7%, 3.3% 47.1% respectively.
As a learner the percentages of student participation in PAL sessions before the exams of 1st MBBS, 2nd MBBS Part 1, 2nd MBBS Part 2 and Final MBBS examinations were 98.7%, 40.4%, 55% and 31% respectively. The student participation for PAL lectures was 86.5%, multiple choice questions 67.6%, structured essay questions 54.7% and clinical case discussions 43.6%.
Most students felt that MCQ discussions (94.2%), clinical case discussions (93.6%) and SEQ discussions (93.9%) were almost equally useful as lectures (91.4%).
Throughout the five years, the majority of the students’ frequency of attendance for the PAL sessions conducted for the main exams was in the range of 1-2 times a week to less than once a month. However, 33.8% of students had never attended PAL sessions before the 2nd MBBS part 2 examination in the fourth year.
The tutors for the PAL session were a batch mate, a senior colleague or an immediate graduate. The senior colleague was the common tutor up to 2nd MBBS Part 2 and an immediate graduate was the common tutor for the final exam.
Physiology (90.7%), followed by Anatomy (88.1%), Community Medicine (59.6%) and Biochemistry (52.3%) were the subjects to which most attended a PAL session. The attendances for Forensic Medicine, Family Medicine and Obstetrics and Gynaecology were lowest at 6%, 4.7%, and 2.6 % respectively.
Most students felt that during the following exam, PAL sessions should be conducted 1-3 months before 1st MBBS (44.4%), 2nd MBBS Part 1 (34.6%) and 2nd MBBS Part 2 (37.3%). In the final year most students (30.7%) felt that PAL should be conducted 1-2/ weekly and daily for the repeat examination. Most students felt that peer teaching could improve their knowledge (86.5%), teaching skills (85.9%), and communication skills (82.4%). In addition, they think it helps to pass examinations (93.9%) and to build up a good relationship with junior colleagues (65.9%) ( p<0.01). Students felt that PAL should be included in the formal curriculum and further provided numerous benefits as listed in Table 1.
When asked about the preferred media of instruction of PAL sessions, 68.4% felt that it should be conducted in both Sinhala and English whereas 21.6% preferred it to be conducted only in Sinhala and 9.9% only in English.
Discussion
The comprehensive analysis of peer-assisted learning (PAL) participation and preferences among medical students reveals compelling insights into its widespread adoption and perceived effectiveness.
To comment on the participation pattern an overwhelming majority of students (99.3%) have engaged with PAL at some point in their medical career, either as learners, tutors, or both. The diverse participation modes, with nearly half of the students engaging in PAL as both learners and tutors, underscore its integral role in the medical education landscape.
The distribution of student participation in PAL sessions before various examinations provides valuable context. The high involvement before 1st MBBS exams indicates its perceived importance in foundational learning, while variations in participation across subsequent years suggest evolving study strategies. Notably, a substantial percentage of students had not attended PAL sessions before 2nd MBBS Part 2, highlighting potential gaps in engagement during this critical period.
The variance in attendance across different subjects signifies varying student preferences and perceived challenges. Physiology and Anatomy emerge as the most attended PAL sessions, reflecting their perceived complexity. Conversely, lower attendance in certain specialties may indicate areas where students feel less need for collaborative learning or potential curriculum gaps.
The students’ overwhelmingly positive perception of PAL sessions as equally beneficial as traditional lectures underscores the effectiveness of this pedagogical approach. Notably, MCQ discussions, clinical case discussions, and SEQ discussions are perceived as highly valuable, emphasizing the diverse benefits PAL offers in different learning contexts.
The frequency preferences for PAL sessions before different examinations reflect nuanced student needs throughout their academic journey. The variability in preferences suggests the importance of flexible PAL scheduling aligned with the academic demands of each phase.
Students acknowledge the multifaceted benefits of PAL, attributing its effectiveness to knowledge enhancement, improved teaching and communication skills, and exam success. The recognition of PAL’s role in fostering positive relationships with junior colleagues underscores its potential impact beyond academic realms.
The diverse preferences regarding the language of instruction for PAL sessions highlight the importance of catering to linguistic diversity among medical students. Striking a balance between Sinhala and English instruction might enhance inclusivity and engagement.
The graphical representation comparing PAL with the formal curriculum suggests a nuanced relationship, indicating that students perceive PAL as a valuable complement rather than a substitute. This aligns with the notion that PAL serves to enrich and reinforce formal learning structures.
The identified qualities expected from PAL teachers underscore the importance of approachability, subject expertise, and effective communication. These attributes align with the student-driven nature of PAL, emphasizing the role of peer educators as facilitators rather than traditional instructors.
Conclusion
PAL is widely accepted and practiced in our medical school. PAL sessions are most sought after at the beginning and the end of the medical course. Most of the students reckon the PAL sessions to be effective in getting through examinations in addition to gaining knowledge. There were hardly any drawbacks from the perspectives of the students towards PAL except for the lack of resources for teaching and learning.
As the majority of the study population feels that the PAL sessions should be encompassed in the formal teaching curriculum, this should be seriously explored further, at higher levels of the curriculum development committee. Supervision the accuracy of knowledge taught at PAL sessions, providing suitable environmental facilities to hold these sessions, training the peer teachers, scrutinizing the study materials, making more model questions available for the discussions and regularizing the present ad-hoc sessions are some of the measures the faculty members could provide to make PAL sessions more useful.
Ethics approval and consent to participate:
Consent and Ethics approval from the research committee of the Colombo South Teaching Hospital. Our study did not include any interventions on participants.
Consent for publication: Consent implied
Availability of data and material: The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Competing interests: No financial or nonfinancial competing interests
Funding: None
Authors’ contributions: NY contributed to the literature search, acquisition of data, analysis of data, interpretation of data, and drafting of manuscript. CP contributed to the literature search, acquisition of data, analysis of data, interpretation of data, and drafting of the manuscript. TK contributed to the literature search, acquisition of data, analysis of data, interpretation of demand, and drafting of the manuscript. JI contributed to the conception and design of the study, revising the manuscript critically for important intellectual content. ATM and SBG contributed literature search, data analysis, drafting of the manuscript and revising the manuscript critically for important intellectual content. SN was involved in data analyses and drafting of the manuscript. All authors read and approved the final manuscript.
List of Abbreviations:
PAL: Peer Assisted Learning
USJP: University of Sri Jayewardenepura
MCQ: Multiple Choice Questions
SEQ: Structured Essay Questions
References
- Topping K, “The effectiveness of peer tutoring in higher and further education: A typology and review of the literature,” Higher Education, vol. 32, pp. 321–345, 1996.
- E. A. B. 1. Tang T, “Learning by Teaching”: A Peer -Teaching Model for University Training in Medical School,” Teaching and Learning in Medicine, vol. 16, pp. 60–63, 2004.
- S. Topping KJ, “Peer-assisted learning,” 1998.
- Hill, F. Liuzzi, and J. Giles, “Peer-assisted learning from three perspectives: student, tutor and co-ordinator,” Clin Teach, vol. 7, no. 4, pp. 244–246, Dec. 2010, doi: 10.1111/J.1743-498X.2010.00399.X.
- Bulte, A. Betts, K. Garner, and S. Durning, “Student teaching: views of student near-peer teachers and learners,” Med Teach, vol. 29, no. 6, pp. 583–590, Jul. 2007, doi:10.1080/01421590701583824.
- Zhang and M. Maconochie, “A meta analysis of peer-assisted learning on examination performance in clinical knowledge and skills education,” BMC Med Educ, vol. 22, no. 1, Dec. 2022, doi:10.1186/s12909-022-03183-3.
- Kommalage and H. Thabrew, “Student-led Peer-assisted Learning: The Kuppi Experience at the Medical School of the University of Ruhuna in Sri Lanka,” 2011. [Online]. Available: http://www.educationforhealth.net/
- “Peer-assisted learning in the UCL Medical School | Teaching & Learning – UCL – University College London.” Accessed: Mar. 07, 2024. [Online]. Available: https://www.ucl.ac.uk/teaching-learning/casestudies/2014/jun/peer-assisted-learning-uclmedical-school
- Bradley, M. A. Fischer, J. Bradley, and M. M. E. Fischer, “Are Our Students Teachers?,” May 2022, doi: 10.13028/3NWB-3A23.
- M. Lockspeiser, P. O’ Sullivan, A. Teherani, and J. Muller, “Understanding the experience of being taught by peers: the value of social and cognitive congruence,” Adv Health Sci Educ Theory Pract, vol. 13, no. 3, pp. 361–372, Aug. 2008, doi: 10.1007/S10459-006-9049-8.
- G. Tolsgaard, A. Gustafsson, M. B. Rasmussen, P. Hoiby, C. Muller, and C. Ringsted, “Student teachers can be as good as associate professors in teaching clinical skills,” Med Teach, vol. 29, no. 6, pp. 553–557, Jul. 2007, doi: 10.1080/01421590701682550.
- D. Peets et al., “Involvement in teaching improves learning in medical students: A randomized cross-over study,” BMC Med Educ, vol. 9, no. 1, pp. 1–5, Aug. 2009, doi:10.1186/1472-6920-9-55/FIGURES/2.