Medical Journal
Published by
Faculty of Medical Sciences,
University of Sri Jayewardenepura,
Nugegoda,
Sri Lanka.
Original Articles
Knowledge of insulin therapy, emergency management, chronic complications and their associated factors among adult patients with type 1 diabetes attending the National Diabetes Centre - Rajagiriya
Hathurusinghe HDWP1*, Saranga MAI1, Mylvaganam P1, Nirmanie GN1, Weeratunga CS1, Arambewela MH2, Wijesuriya M3, Goonewardena CSE4,5
1Faculty of Medical Sciences, University of Sri Jayewardenepura
2Department of Physiology, Faculty of Medical Sciences, University of Sri Jayewardenepura
3Director, National Diabetes Centre, Rajagiriya
4Department of Community Medicine, Faculty of Medical Sciences, University of Sri Jayewardenepura
5Non Communicable Disease Research Centre, University of Sri Jayewardenepura
*wisalprasastha5414@gmail.com
Abstract
Introduction: Type 1 diabetes mellitus (T1DM) is a growing concern in Sri Lanka and preventing long-term disease-related complications and reducing the frequency of emergency management of episodes is a challenge for these patients.
Objectives: To describe the knowledge on insulin therapy, emergency management, chronic complications and their associated factors among adult patients with T1DM attending National Diabetes Center – Rajagiriya.
Results: The majority (70%) were between 18-27 years of age with a mean age of 25.54 years (SD=5.690). The age of disease onset was less than 15 years among 82% of patients. Mean Knowledge scores on chronic complications, insulin therapy and emergency management were 81.49(SD=0.5) 67.76(SD=0.49), 42.92(SD=0.5) respectively. Those with higher education had better knowledge of insulin therapy, chronic complications and emergency management (p<0.05).
Conclusions: The majority had satisfactory knowledge scores for insulin therapy and chronic complications but poor knowledge scores for emergency management. Therefore, patient education, awareness and empowerment on more specific issues related to the emergency management of this lifelong disease is beneficial.
Keywords: Type 1 Diabetes patients, knowledge, insulin therapy, chronic complications, emergency management
Introduction
Type 1 diabetes mellitus (T1DM), also known as autoimmune diabetes, is a chronic disease characterized by insulin deficiency due to pancreatic β-cell loss and leads to hyperglycaemia. Although the age of symptomatic onset is usually during childhood or adolescence, symptoms can sometimes develop much later. Although the aetiology of T1DM is not completely understood, the pathogenesis of the disease is thought to involve T cell-mediated destruction of β-cells [1].
Type 1 diabetes (T1DM) is usually diagnosed before the age of 40, although occasionally people have been diagnosed later after an illness which causes the immune response to trigger it. According to the data of the National Diabetes Centre in Sri Lanka, out of the 672 patients, the age at diagnosis ranged from birth to 44 years, and the majority of patients, 526 (78.3%) were diagnosed before 15 years of age [2].
Chronic complications in T1DM can be broadly categorised as microvascular and macrovascular. Microvascular complications include mainly diabetic kidney disease, neuropathy, and retinopathy. Poor glycaemic control and longer duration of diabetes are the most important determinants of microvascular complications in Type 1 diabetes. According to t medical reports in Denmark, the prevalence of moderate to severe retinopathy ranged from 23%–59% while the prevalence of neuropathy ranged from around 30%–60% and diabetic kidney disease defined as micro or microalbuminuria affected up to 30% of persons with Type 1 diabetes. Macrovascular complications include mainly coronary artery disease, peripheral artery disease, and stroke. Most of the macrovascular complications are associated with atherosclerotic plaque formation due to impairment of lipid metabolism [3].
Diabetic ketoacidosis (DKA) is a common but potentially fatal medical emergency among people with type 1 Diabetes mellitus, there are ~6000 episodes per year in the UK. [4].
Fifteen to sixty-seven per cent of patients with new-onset type 1 diabetes mellitus (T1DM) present with diabetic ketoacidosis (DKA), of which approximately 79%, initially present to their general practitioner.
Diabetic ketoacidosis is the most common cause of diabetes-related deaths, mainly due to cerebral oedema that occurs in 0.3-1% of patients. Measurement of ketone bodies is recommended for patients with T1DM during acute illness when blood glucose is elevated above 300 mg/dl or when patients have signs of ketoacidosis. Treatment of DKA focuses on normalising blood glucose and treating precipitating factors to prevent a recurrence [5].
Methodology
A descriptive cross-sectional study was conducted among 228 people above 18 years with T1DM, on treatment for at least one year duration attending National Diabetic Center – Rajagiriya from November 2020 to May 2021. Those with physical and mental disability were excluded. The sample size was calculated using the formula for estimation of proportions in descriptive studies [7]. A standard normal deviation for specified alpha error was set at 1.96 which corresponds to 95%, while precision was set at 0.05. The proportion of adequate knowledge of the T1DM in adolescents with longer the time of diagnosis was 26% [8]. With a non-response of 5%, the final sample size was 326. Patients who fulfilled the inclusion criteria and who attended the clinic during the study period were selected.
Self-administered questionnaires were circulated as Google Forms which was designed after the face validity by the Endocrinologist. Data was collected through printed questionnaires from patients attending the clinic while for those not attending the clinic due to COVID restrictions, Google forms were used. Each correct statement of knowledge was given 1 mark and zero for incorrect/ don’t know the response. Knowledge score was categorised using the mean knowledge. Those who scored above mean as good knowledge and those below mean score as poor knowledge. Descriptive statistics were performed and analysed, and their associations were established using the chi-square test from the SPSS software version 23. P<0.05 was taken as the significance level.
Hypoglycemia is defined as blood glucose < 70 mg/dl. The annual prevalence of severe Hypoglycaemia is around 30% in people with type 1 DM [6].
Structured training in insulin self-management reduces both rates of ketoacidosis and severe hypoglycaemia, requiring emergency treatment. This study reinforces the importance of making high-quality structured education more readily available to people with type 1 DM [4]. There is scarce research done among T1DM patients to assess their knowledge regarding the disease, insulin treatment and emergency management. Thus, this study aimed to describe the knowledge of insulin therapy, emergency management, chronic complications and their associated factors among adult patients with T1DM attending the National Diabetes Centre – Rajagiriya.
Results:
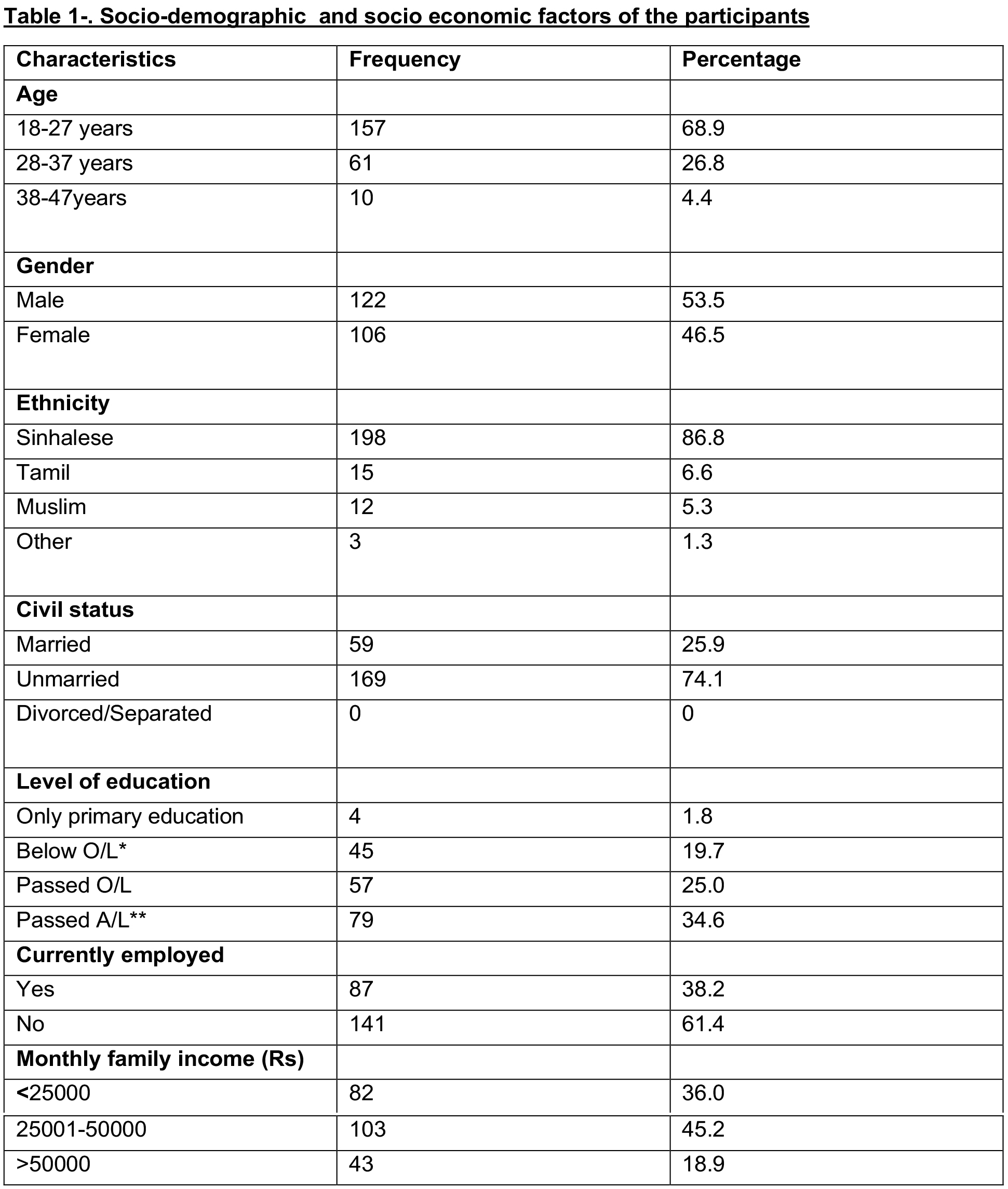
The response rate was 77%. (Total sample size-228) The majority (68.9%) were in the 18-27 age group. The mean age of the study population was 25.54 (SD = 5.690) years. The majority of the participants were male (53.5%), unmarried (74.1%) and Sinhalese (86.8%). More than half of the population had passed A/Ls.
The mean age at the time of diagnosis was 10.74 (SD = 4.4449) years. Disease onset was at less than 15 years of age among 82% of the patients (Table 1).
The mean knowledge score of insulin therapy was 62.761(SD =0.49876). The mean knowledge score regarding acute and chronic complications was 42.9247 (SD = 0.50079) and 81.4912 (SD= 0.50041) respectively.
The knowledge was categorised according to the mean score 45.2% had good knowledge of insulin therapy, 48.2% had good knowledge of acute complications and 52.6% had good knowledge of chronic complications of DM (Figure 1).
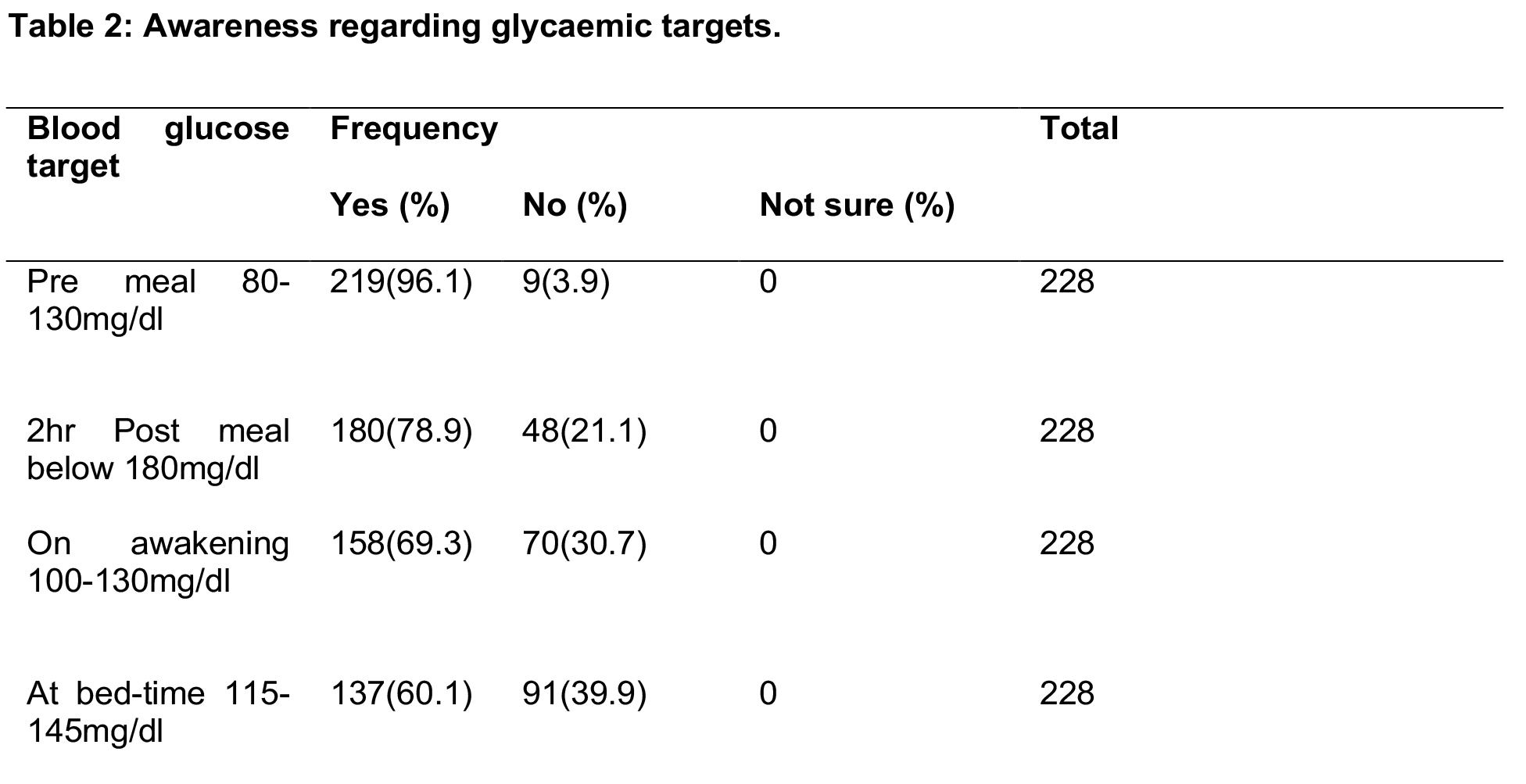
According to Table 2, awareness of glycaemic targets was satisfactory with 96% being aware of their pre-meal blood glucose target of 80-130 mg/dl, 78.9% on postprandial targets, 69.3% on target levels at awakening and 60% of bedtime targets.
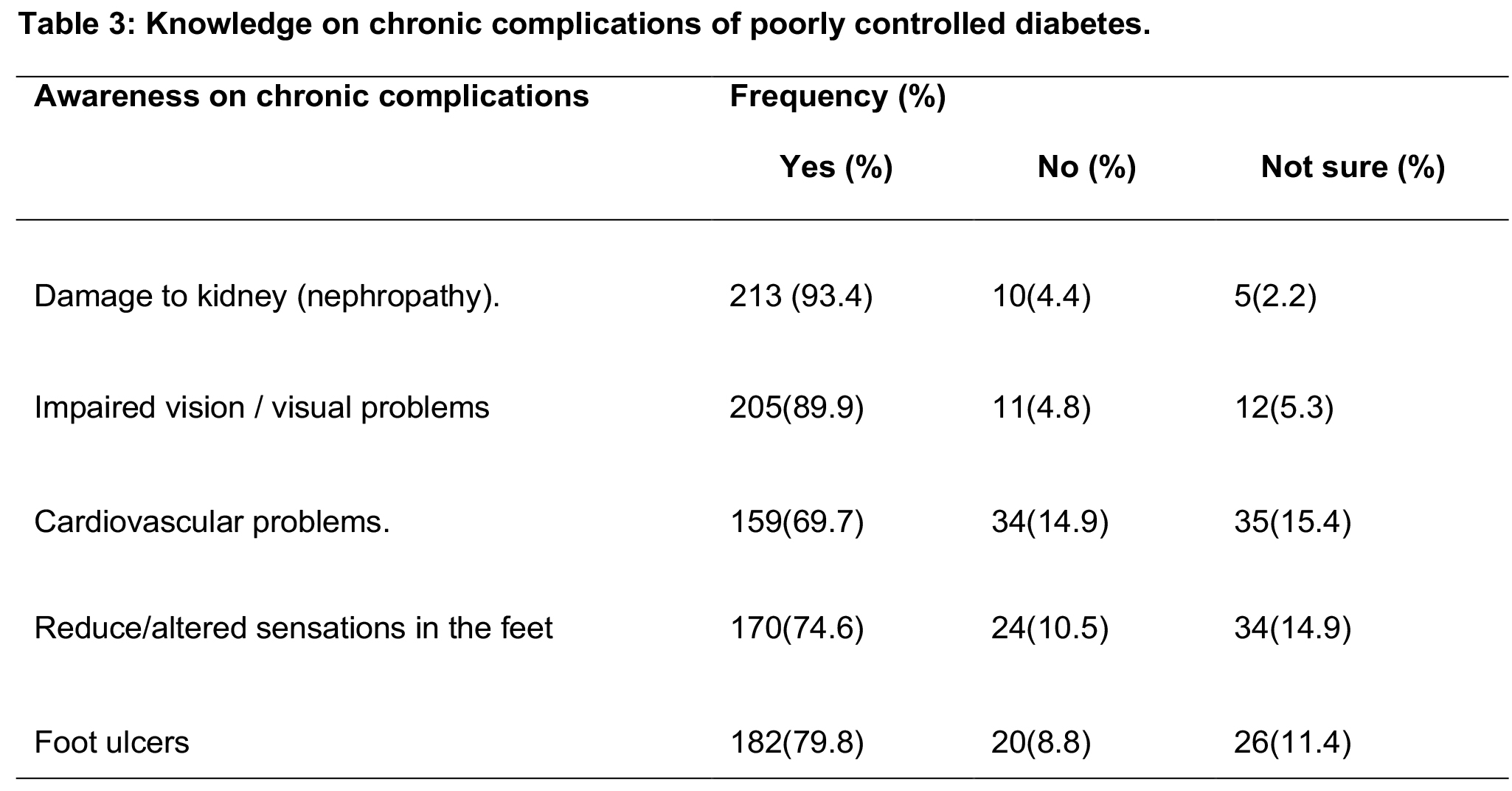
The majority of the participants were aware of the microvascular complications. However, awareness regarding macrovascular complications was less (Table 3).
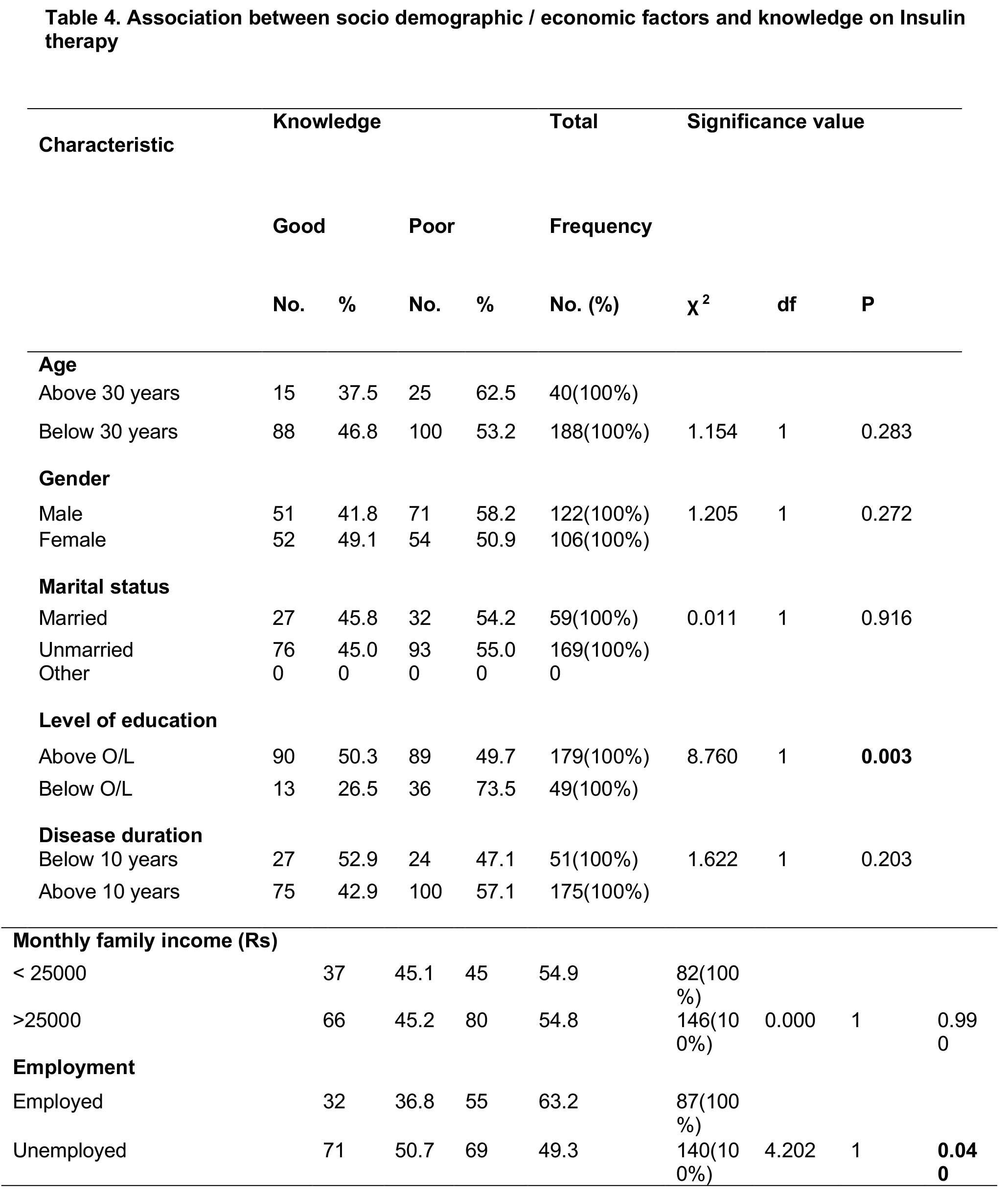
Statistically significant association with good knowledge of insulin therapy was only demonstrated with those having an education above ordinary level (p<0.05). Surprisingly, those who were unemployed had better knowledge compared to those who were employed (50.7% vs 36.8%) and this difference was statistically significant (p<0.05). Other socio-demographic and economic variables did not show any significant association. (Table 4)
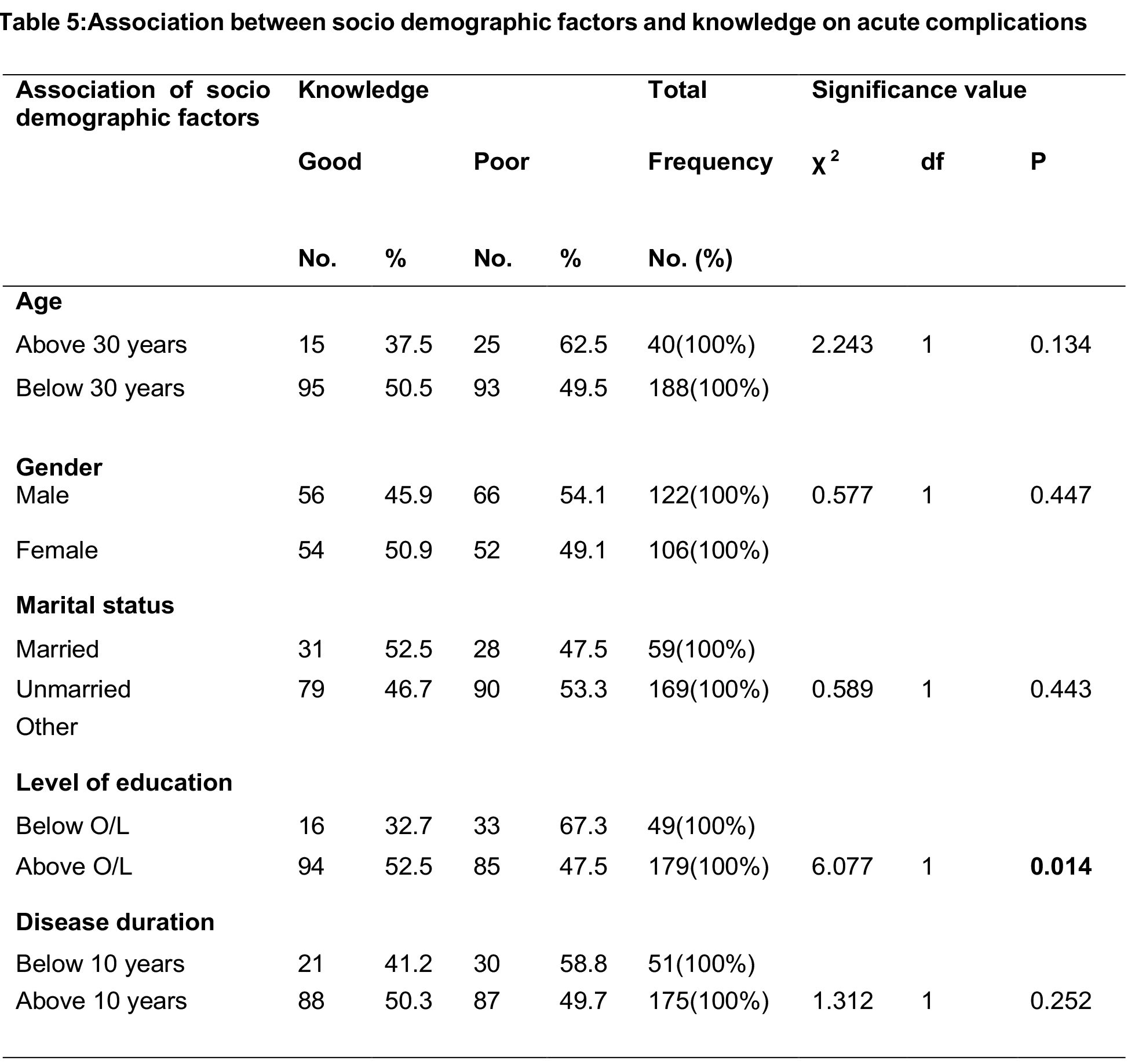
Table 5 depicts the association between sociodemographic factors and knowledge of acute complications. Participants who had an educational level above the ordinary level had better knowledge compared to those who had an educational level below O/L (52.5% vs 32.7%). This observed difference was statistically significant (p<0.05). None of the other factors showed any significant difference (p>0.05).
Discussion
Our study showed that awareness of glycaemic targets was satisfactory with 96%, 78.9%, and 60% being aware of pre-meal, postmeal, and bedtime glycaemic targets. Good knowledge was seen on insulin storage and transportation among 97.8% and 96.1%, respectively. The awareness of the site of insulin injection among the participants is as follows: thigh 57.5%, abdomen 71%, and upper part of the arm 65.8%. In our research findings, 97.8% were aware that insulin should be stored in the middle compartment of the refrigerator.
According to a cross-sectional study conducted by Metu Karl Heinz Referral Hospital in 2019, more than three-fourths (78.9%) answered that insulin injection should be done before taking a meal or just soon after a meal. One hundred sixty-seven (69.0%) correctly answered that sites for insulin injection are the abdomen, thigh, glutei, and deltoid. More than half (56.2%) answered that an insulin vial is stored in the refrigerator or cold place, or sand soaked with water. One hundred eighty-five (76.4%) correctly answered that rotation of the injection site is used to reduce pain and prevent wasting of subcutaneous tissues.
In our study, only 45.2% had a good knowledge of insulin therapy. As a person living with T1DM is dependent on insulin and requires multiple injections per day, these findings highlight the urgent need to educate and train these young people regarding insulin storage, transportation, and injections. A similar study was reported by Yosef et al., where only 38.4% of respondents had a good knowledge of insulin therapy. The sample size for this research was 245.
Our study highlighted good knowledge regarding chronic complications such as diabetic kidney disease, eye disease, and foot disease. The National Diabetic Centre provides an annual assessment of these complications, and therefore, this is likely the reason for increased awareness regarding this complication.
The majority (79%) of patients knew about foot ulcers, and 74.6% of the proportion knew impaired sensation in the feet. The least (69.7%) known chronic complication among study participants was cardiovascular complications. As this is a young patient population and may not have undergone regular screening for cardiovascular disease, this perhaps may have caused less awareness regarding this important complication. However, as cardiovascular disease is one of the leading causes of mortality among these patients, more awareness must be created. Contrasting results were observed in a similar study done in Ghana, where the knowledge of these complications was quite low.
In our research, knowledge of chronic complications of T1DM had the highest mean score, and 52.6% of patients had good knowledge. A cross-sectional study conducted in the Medical B Unit of the Department of Medicine Khyber Teaching Hospital, Peshawar among 96 patients reported only 36 (37.50%) had good, 24 (25%) had average, and 36 (37.50%) had poor knowledge about diabetes complications. In this study, they had categorized the knowledge of complications into three parts, whereas in our study, two parts. The sample size was low compared to our study.
Our research demonstrated that 51.8% had poor knowledge regarding acute complications, which was scored based on statements regarding symptoms, reasons, and actions to be taken during hypo/hyperglycaemia. However, their knowledge of hypoglycaemia (91.7%) and hyperglycaemia (91.2%) was reported good. This may be because our patients most commonly experienced these two emergencies, and allergies to insulin were rather rare.
In our research, there was no significant association between knowledge of insulin therapy and age. Our findings showed that those who were of higher educational level had better knowledge of insulin therapy, and this was statistically significant. Similar results were obtained by a study done in Metu – Karl Heinz Referral Hospital from January 01-30, 2019, in Ethiopia, where the respondents who achieved secondary school and above had three times increased odds of having good knowledge of insulin therapy.
In our research, there were no significant differences with gender or marital status. When discussing the disease duration, our findings demonstrated that for the participants who used insulin below ten years, 52.9% of participants had a good knowledge, while 42.9% of participants who used insulin above ten years had a good knowledge. However, there was no significant association between knowledge of insulin therapy and the disease duration. In contrast, research done in Ethiopia had 3.7 times increased odds of having good knowledge of insulin therapy than those who used insulin for less than five years. The difference observed in our study and the abovementioned study was probably due to our sample having a higher percentage of participants below 30 years.
In our study, the results showed that those who were unemployed had a better knowledge of insulin therapy compared to those who were employed. This might be due to a high proportion who have finished their exams and may be looking for a job and will fall under the unemployed category, whereas those who have dropped out of school are employed in small jobs.
Limitations:
Due to the COVID-19 pandemic, only a few patients came to the National Diabetes Centre. The response rate on WhatsApp and Google Forms was also limited. The mean knowledge scores were calculated based on their mean knowledge score. Therefore, the reduced sample size may have affected the results.
Conclusions:
The majority of the participants (52.6%) had a good knowledge of chronic complications of T1DM. However, the majority of the patients had poor knowledge of insulin therapy (54.8%) and acute complications management (51.8%). However, patients who had been educated above ordinary levels had significantly better knowledge (p<0.05) on insulin therapy, acute complications, and better overall knowledge of T1DM. There was no significant difference between the level of education and knowledge of chronic complications. Unemployed patients had better knowledge of insulin therapy compared to employed patients, and this association was statistically significant (p<0.05).
Recommendations:
To increase patient education and awareness on more specific issues related to T1DM, such as insulin storage, administration, recognizing warning symptoms, initial self management, and when to seek urgent medical attention during acute complications such as hypoglycaemia and diabetic ketoacidosis. This will help empower patients with this lifelong disease to self-manage their disease condition more optimally.
Acknowledgements:
We would like to acknowledge the National Diabetic Centre, Rajagiriya, for all the support given to us during the data collection period with the COVID restrictions. We also wish to thank all the patients who participated in this research.
Conflicts of Interest:
There is nothing to declare.
References
- Katsarou A, Gudbjornsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, Jacobsen LM, Schatz DA, Lernmark A. Type 1 diabetes mellitus. Nat Rev Dis Primers. 2017 Mar 30;3:17016. doi: 10.1038/nrdp.2017.16. PMID: 28358037.
- Wijesuriya MA, Sandy JL, Warnapura CL, Middlehurst AC, Ogle GD. Characteristics of insulin registry patients with Type 1 diabetes in Sri Lanka. J Diabetol 2019;10:37-40
- Bjerg L, Hulman A, Charles M, Jorgensen ME, Witte DR. Clustering of microvascular complications in Type 1 diabetes mellitus. J Diabetes Complications. 2018 Apr;32(4):393-399. doi: 10.1016/j.jdiacomp.2018.01.011. Epub 2018 Feb 22. PMID: 29478814.
- Elliott J, Jacques RM, Kruger J, Campbell MJ, Amiel SA, Mansell P, Speight J, Brennan A, Heller SR. Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with Type 1 diabetes. Diabet Med. 2014 Jul;31(7):847-53. doi:10.1111/dme.12441. Epub 2014 Apr 8. PMID:24654672; PMCID: PMC4264891.
- Siafarikas A, O’Connell S. Type 1 diabetes in children – emergency management. Aust Fam Physician. 2010 May;39(5):290-3. PMID:20485715.
- Kahanovitz L, Sluss PM, Russell SJ. Type 1 Diabetes – A Clinical Perspective. Point Care. 2017 Mar;16(1):37-40. doi:10.1097/POC.0000000000000125. PMID:28943810; PMCID: PMC5606981.
- Lemeshow S. Sample size determination in health studies: a practical manual. World Health Organization; 1991.
- Moskovitz A, Alex Knee M, Frydman E, Allen H, Tonyushkina K. Diabetes knowledge in youth with T1DM and their caregivers-a crosssectional study. J Diabetes Clin Prac. 2018;1(1):101.
- Yosef T. Knowledge and Attitude on Insulin Self-Administration among Type 1 Diabetic Patients at Metu Karl Referral Hospital, Ethiopia. J Diabetes Res. 2019 Dec 14;2019:7801367. doi: 10.1155/2019/7801367. PMID: 31915711; PMCID: PMC6935447.
- Obirikorang, Y., Obirikorang, C., Anto, E.O. et al. Knowledge of complications of diabetes mellitus among patients visiting the diabetes clinic at Sampa Government Hospital, Ghana: a descriptive study. BMC Public Health 16, 637 (2016). https://doi.org/10.1186/s12889-016-3311-7
- Ullah F, Afridi AK, Rahim F, Ashfaq M, Khan S, Shabbier G, Rahman SU. KNOWLEDGE OF DIABETIC COMPLICATIONS IN PATIENTS WITH DIABETES MELLITUS. J Ayub Med Coll Abbottabad. 2015 Apr-Jun;27(2):360-3. PMID: 26411116.
- Nasir BB, Buseir MS, Muhammed OS. Knowledge, attitude and practice towards insulin self-administration and associated factors among diabetic patients at Zewditu Memorial Hospital, Ethiopia. PLoS One. 2021 Feb 8;16(2):e0246741. doi: 10.1371/journal.pone.0246741. PMID: 33556090; PMCID: PMC7870072.
- Gulabani M, John M, Isaac R. Knowledge of diabetes, its treatment and complications amongst diabetic patients in a tertiary care hospital. Indian J Community Med. 2008 Jul;33(3):204-6. doi: 10.4103/0970-0218.42068. PMID: 19876488; PMCID: PMC2763678.
- l-Hadhrami R, Al-Rawajfah O, Muliira J. Diabetes Self-Management and the Associated Factors Among Adult Omanis with Type 1 Diabetes. Sultan Qaboos Univ Med J. 2020 Nov;20(4):e339-e345. doi:10.18295/squmj.2020.20.04.010. Epub 2020 Dec 21. PMID: 33414939; PMCID: PMC7757915.