Medical Journal
Published by
Faculty of Medical Sciences,
University of Sri Jayewardenepura,
Nugegoda,
Sri Lanka.
Original Articles
Child Sexual Abuse: Maternal Knowledge, Consequences and Prevention Strategies in Child Welfare Clinics of Southern Sri Lanka
Hasinika APD1, Dhammearatchi K2, Ariyarathne HTDW3
1Department of Nursing and Midwifery, Faculty of Allied Health Sciences, University of Sri Jayewardenepura.
2Faculty of Medical Sciences, University of Sri Jayewardenepura
3Department of Forensic Medicine, Faculty of Medical Sciences, University of Sri Jayewardenepura
Abstract
Introduction: Child sexual abuse (CSA) is a grave violation involving any sexual activity with a child by an adult or older adolescent causing profound physical and psychological trauma.
Objectives: The objective was to investigate knowledge, consequences and prevention strategies implemented against CSA among mothers as the primary caretakers of young children.
Methods: A descriptive cross-sectional study was conducted in two Medical Officer of Health areas in Matara district, Sri Lanka among 106 mothers who attended child welfare clinics. An interviewer administered questionnaire was used.
Results: 51.9% of mothers had a good level of knowledge while 24.5% were poor. Mothers who had passed A/L, and those who had both male and female children were more knowledgeable regarding CSA. 89.6% were aware that both sexes were abused. Bleeding from the genital tract (93.4%) and getting pregnant (93.4%) were identified as the main physical consequences of CSA. Bed wetting or faecal passing beyond the usual age (29.2%) was poorly understood. Developing phobias (95.3%), troubled school performance (92.5%) and avoiding the opposite sex (84.9%) were identified as the main psychological consequences. Educating the child (96.2%), being vigilant regarding the child’s physical (100%) and behavioural (100%) changes were the most common prevention strategies practiced. Most vulnerable situations identified were the school van (90.5%) and tuition classes (86.7%).
Conclusions: Knowledge and awareness of specific consequences of CSA was inadequate. Implementation of public health education programmes are recommended to both educate and empower society.
Introduction
Child sexual abuse (CSA) is a grave violation involving any sexual activity with a child by an adult or older adolescent causing profound physical and psychological trauma. Child Sexual abuse is defined as the involvement of a child in sexual activity that he or she does not fully comprehend, is unable to give informed consent to, or for which the child is not developmentally prepared, or else that violates the laws or social taboos of society [1]. This abuse can take various forms, including physical contact, exploitation, and exposure to inappropriate material. Initial effects such as fear, anxiety, depression, anger and hostility, aggression, and sexually inappropriate behaviour are well documented [2]. These sequelae are even more consequential as children subjected to such atrocious behaviour undoubtedly undergo long term ramifications. Frequently reported long-term effects include depression and self-destructive behaviour, anxiety, feelings of isolation and stigma, poor self-esteem, difficulty in trusting others, a tendency toward revictimization, substance abuse, and sexual maladjustment [2]. The prevalence of CSA highlights the urgent need for effective prevention and intervention strategies. The scrutiny of this matter is of utmost relevance to a country such as Sri Lanka steeped in traditionalism where certain topics are considered taboo and repressed. This burden weighs heavy on being outspoken and seeking help which is already emotionally and culturally challenging.
There are many supportive services established for sexually abused children available in Sri Lanka. UNICEF Sri Lanka and the Ministry of Women and Children Affairs (MWCA) play a significant role in combating child sexual abuse and other forms of violence against children. Additionally, civil societies, Non-government Organizations (NGOs), and religious institutions provide their support to end violence against children.
The prevalence of CSA highlights the urgent need for effective prevention and intervention strategies. Awareness and education play pivotal roles in combating this issue, particularly among key caregivers such as parents and educators. Mothers, as primary caregivers, are in a crucial position to detect early signs of abuse and take preventive measures. Therefore, understanding their level knowledge and awareness about CSA, along with the strategies they employ to protect their children, is essential for developing targeted educational and support programs.
Methods
A descriptive cross-sectional study was carried out at the Child Welfare Clinics of two randomly selected Medical Officer of Health (MOH) areas in the Matara district located in the Southern province of Sri Lanka. Mothers who attended the clinics with their children were selected via systematic sampling from the registry of clinic patients. Sample size was calculated utilizing the Cochran formula which is a standard formula used in descriptive studies. A sample of 106 participants was obtained. Mothers who had been subjected to CSA personally in the past or had children who had undergone CSA were excluded.
The interviewer-administered questionnaire was developed under the guidance of a Consultant Forensic Physician and influenced by similar studies in South India [3]. It comprised of the following sections.
Section 1: Demographic data (Mother and their child)
Section 2: Knowledge of mothers as to what encompasses as child sexual abuse
Section 3: Mothers’ awareness regarding consequences of CSA
Section 4: Practised preventive strategies against child sexual abuse
Each correctly answered question was given a score of ‘1’, while incorrect responses were given a score of ‘0’. Section 2 consisted of 19 questions while section 3 was divided into two subsections to assess both physical and psychological consequences of CSA. Physical consequences were assessed using 14 questions and 13 questions were used to assess psychological consequences. 12 questions were devoted to assessing the preventive strategies implemented against CSA in section 4.
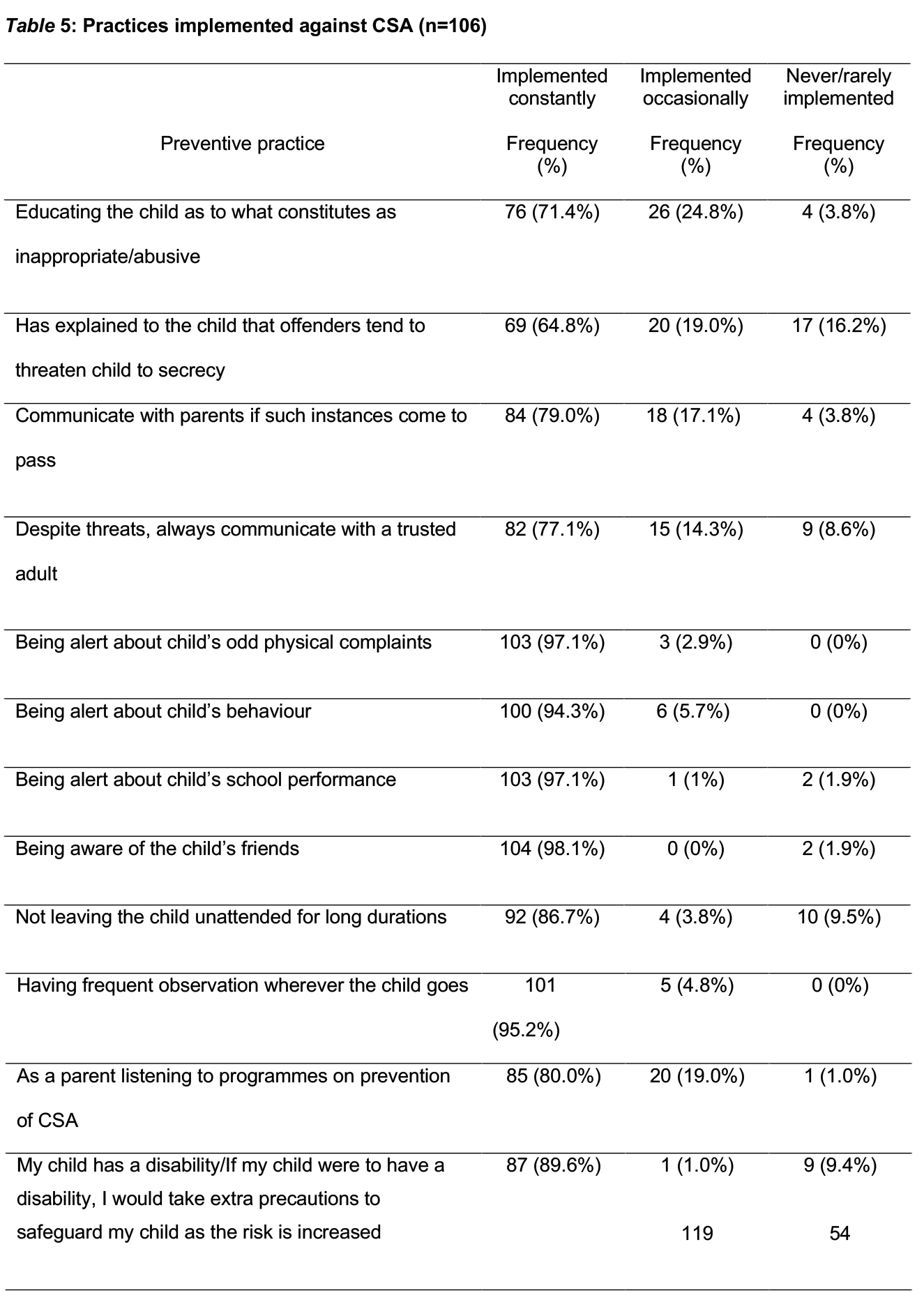
A score equal to or more than 60% was considered as ‘Good knowledge’, a score between 30% and 59% was considered as ‘Satisfactory knowledge’ and a score equal to or less than 29% was considered as ‘Poor knowledge’. Same percentages were used when analysing awareness on consequences of CSA. Implemented preventive strategies against CSA was assessed under 3 measurements, namely, ‘Implemented constantly’, ‘Implemented Occasionally’ and ‘Never/rarely implemented’ and presented using percentages.
Ethical approval was obtained from the Ethics Review Committee of the Faculty of Medical Sciences, University of Sri Jayewardenepura. Administrative approval was obtained from the Regional Director of Health, Matara District under whose purview the two MOH areas fall. Furthermore, the respective Medical Officers of Health approved the research. Informed written consent was obtained prior to administering the interviewer-administered-questionnaire.
Confidentiality and anonymity were ensured and notified via comprehensive information sheets. No data which personally identified the participants was collected. The data was used only for research purposes and participants were made aware of their ability to withdraw from the study at any time.
Result
The final sample amounted to 106 mothers. The results were analysed under four separate sections: socio-demographic characteristics, knowledge of CSA, the awareness of consequences of CSA and practiced precautions against CSA.
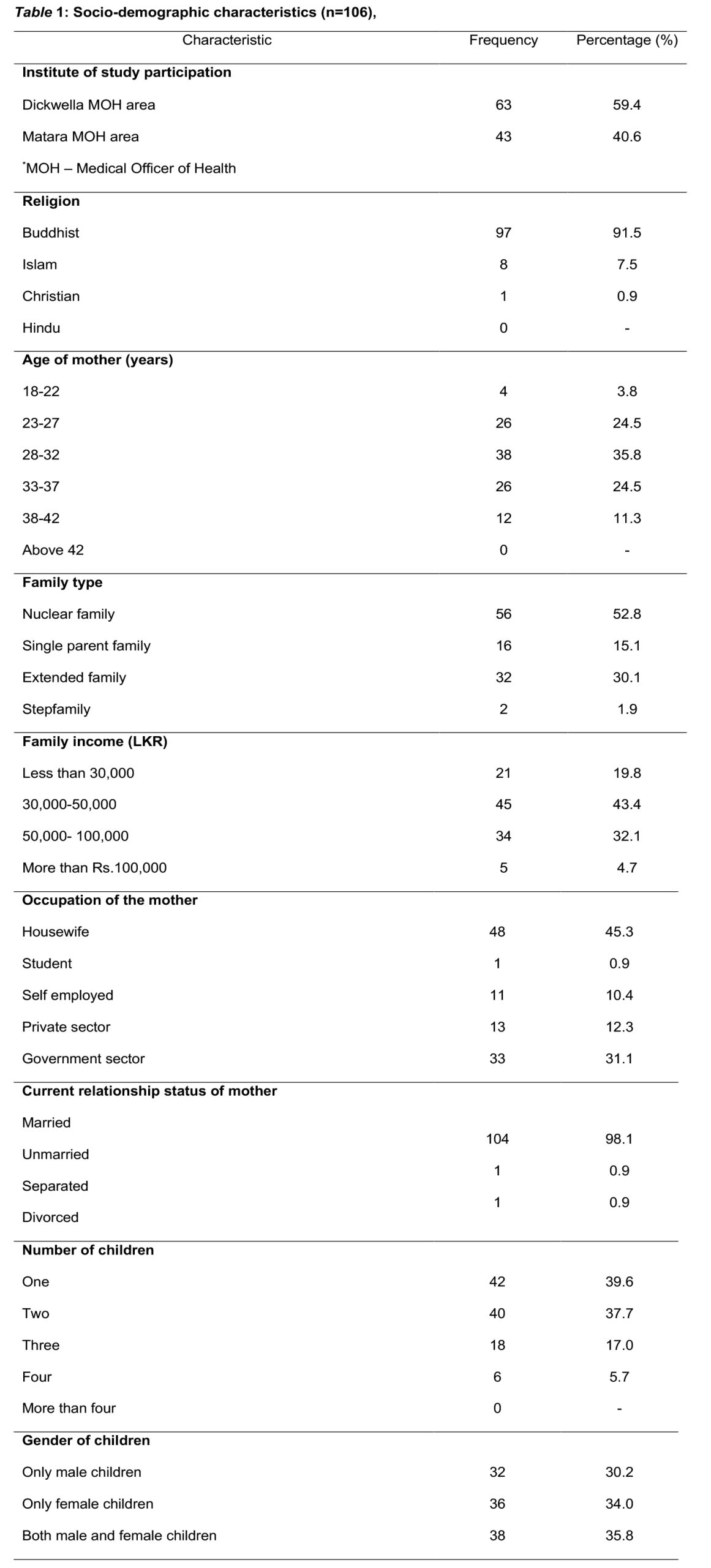
The vast majority of participants were Buddhist (91.5%). The majority were between 28-32 years of age (35.8%). More than half were part of nuclear families (52.8%). The majority of the sample population were unemployed (45.3%). A majority had passed advanced level examination (44.3%) while one respondent (0.9%) had received no school education. An approximately equal proportion had passed ordinary level examination (24.5%) and were educated up to a degree level (22.6%). The majority were currently married (98.1%). The sample consisted of a majority of families that had one child (39.6%); 37.7% of families had two children; 17.0% of families had three children and 5.7% families had four children. Approximately a third each of the sample families had only male children (30.2%), had only female children (34.0%) and had both male and female children (35.8%).
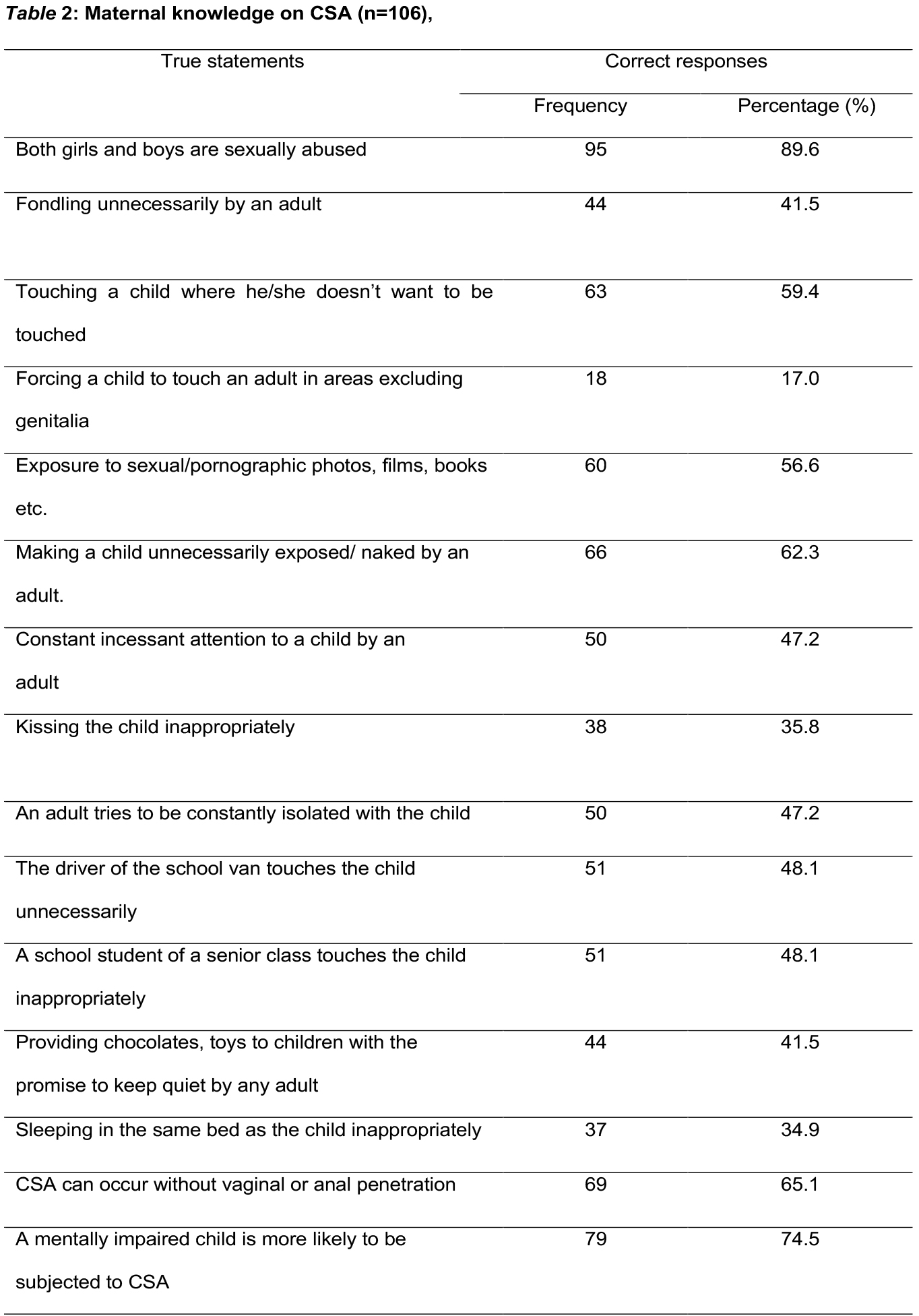
A majority of the sample (89.6%) accurately responded that both boys and girls were subjected to sexual abuse. However, a mere 41.5% identified fondling of the child by an adult could amount to CSA. A surprisingly low portion of the sample (17%) perceived forcing a child to touch an adult in areas excluding genitalia amounted to CSA. A slight majority of the sample (56.6%) accurately responded that exposing a child to sexual or pornographic material was a form of CSA. Almost two thirds of the sample population (62.3%) recognised that unnecessary exposure of the child amounted to abuse. A surprisingly low percentage of the sample (41.5%) accurately responded that bribing the child with toys or chocolates to be quiet about the past was alarming. Only two thirds of respondents (65.1%) accurately recognised that CSA could occur without vaginal or anal penetration. Three out of four respondents (74.5%) were aware that a mentally impaired child was more likely to be subjected to CSA.
The majority of mothers believed that the school van (91.4%), the environment of the village (85.7%) and the school environment (67.6%) were the common settings for being sexually abused. A significant 43.8% of the sample population accepted the possibility of their child/children to be sexually abused at their own house.
Analysis of study findings revealed that just half of the mothers (51.9%) had a good level of knowledge regarding CSA while 23.6% of mothers had satisfactory knowledge and an alarming 24.5% of mothers had poor knowledge regarding CSA.
Upon further analysis of the mothers with a good level of knowledge, those who had completed their O/L’s, mothers aged 28-32, and those who had both male and female children were found to be more knowledgeable.
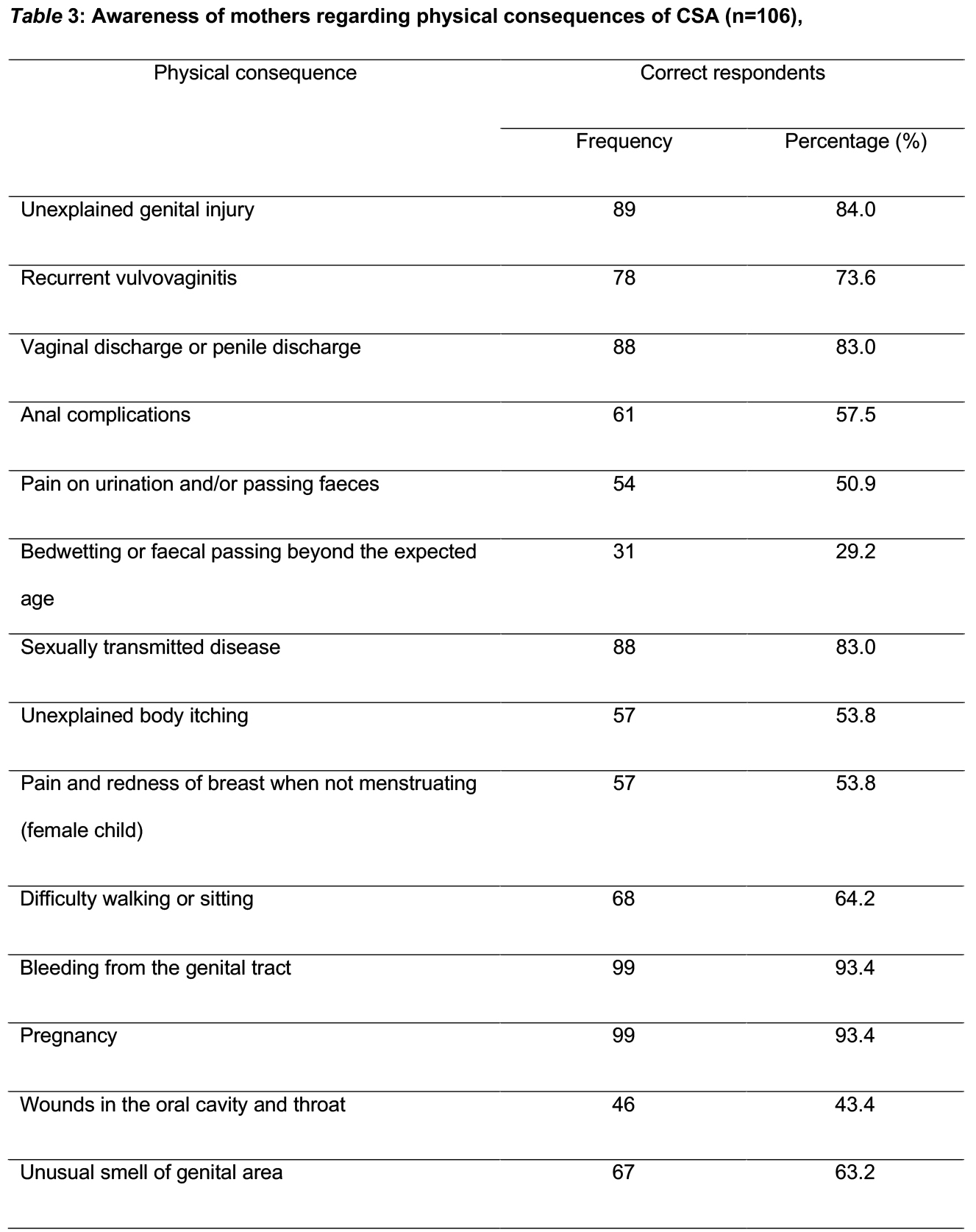
A few specific physical consequences were relatively unrecognized by the sample population. Bedwetting ad faecal passing beyond the expected age (29.2%), wounds in the oral cavity and throat (43.4%) were such consequences. Only half of the respondents were aware that pain upon urination or defaecation (50.9%), unexplained body itching (53.8%), pain or redness of the breast when not menstruating (53.8%) were physical consequences of sexual abuse.
Almost two thirds of mothers (62.3%) had a good level of awareness regarding physical consequences of CSA while 25.5% had a satisfactory level of awareness and 12.3% of the mothers had a poor level of awareness
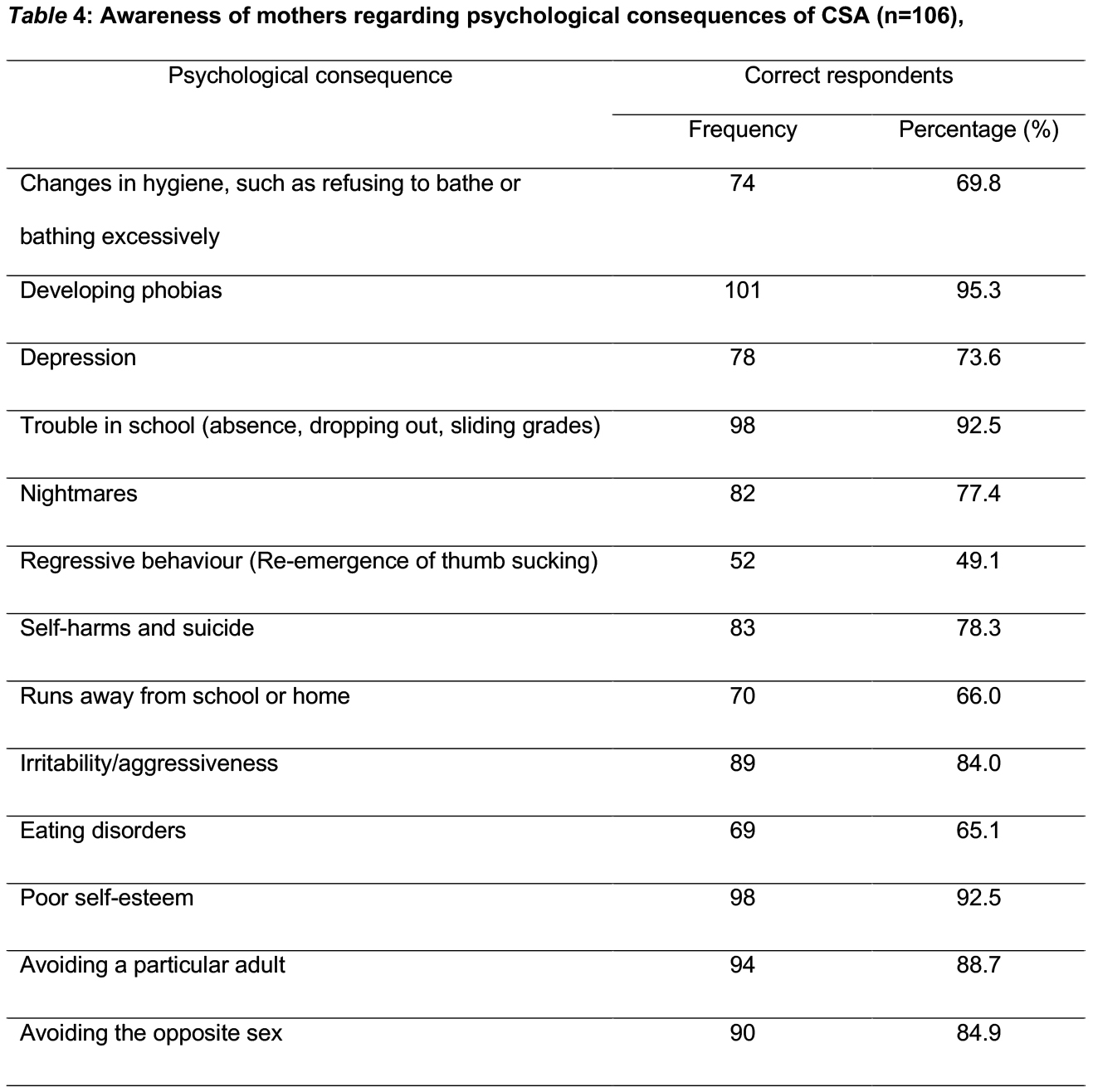
Psychological consequences were quite well understood throughout the sample population. The only less aware consequence was the appearance of regressive behaviours which only 49.1% were aware of.
A significant majority of the sample population (89.6%) had a good level of awareness regarding psychological consequences which can be observed in an abused child while 5.7% of mothers had a satisfactory level of awareness and 4.7% of mothers had a poor level of awareness.
The majority of preventive practices were implemented constantly. A surprising 16.2% of mothers rarely/didn’t educate their children that offenders will threaten the child to secrecy following inappropriate/abusive behaviour. The majority of mothers (86.2%) constantly implemented preventive strategies while 9.45% implemented them occasionally and 4.35% never/rarely implemented any preventive strategies against CSA.
Discussion
Analysis of the current study findings revealed that just half of the mothers (51.9%) had a good level of knowledge regarding CSA while 23.6% of mothers had satisfactory knowledge and an alarming 24.5% of mothers had poor knowledge regarding CSA. A cross-sectional survey involving 400 randomly selected parents attending a Primary Health Care Centre in Saudi Arabia revealed that most respondents (69%) had good knowledge of sexual abuse in children [4].
A study conducted among health care professionals on the concept of child abuse in the Jaffna district of Sri Lanka using 246 participants revealed that all the groups of professionals correctly identified every form of child abuse and 61.7% had correctly identified the social indictors of child abuse [5]. This is welcome research finding since healthcare professionals being more knowledgeable of CSA is of utmost importance when compared to knowledge rates of parents. A majority of the current study sample (89.6%) accurately responded that both boys and girls were subjected to sexual abuse. Similarly, a study which was conducted in Jordan among 488 mothers revealed that 93.9% of Jordanian mothers were aware that boys were also likely to be subjected to sexual abuse [6]. This is an important finding in both cultural contexts since being unaware of sexual abuse experienced by young boys would be extremely damaging to society.
A mere 41.5% of the current study population identified that fondling of the child by an adult could amount to CSA. A surprisingly low portion of the current sample (17%) perceived forcing a child to touch an adult in areas excluding genitalia amounted to CSA. A slight majority of the current sample (56.6%) accurately responded that exposing a child to sexual or pornographic material was a form of CSA. Almost two thirds of the sample population (62.3%) recognised that unnecessary exposure of the child amounted to abuse. A systematic review discovered that the kinds of abuse that appeared to be the most damaging were experiences involving father figures, genital contact, and force [7].
A significant 43.8% of the current sample population accepted the possibility of their child/children to be sexually abused at their own house. A similar proportion of pre-school teachers (50%) reported that CSA can be perpetrated by close family members. However, 72% of teachers reported that CSA prevention programs would induce too much of knowledge about sex [8]. This relates to the important notion of developing structured programs in institutions such as preschools which are age appropriate since abusive behaviour cannot be ruled in the home environment. Three out of four respondents of the current study (74.5%) were aware that a mentally impaired child was more likely to be subjected to CSA. Similarly, a study conducted in Tamil Nadu, India revealed that 88.2% of mothers believed that physical and mental disability in children was a risk factor for CSA [3]. This emphasizes the importance of implementing even more stringent safety precautions when it comes to the care of such disabled children.
A cross-sectional study conducted in Jordan found that genital and /or anal injury & unexplained soreness or bruises around genitals were the commonly associated physical symptoms of CSA which were identified by mothers [6]. Similarly, our study yielded that mothers were aware that unexplained genital injury (84%), anal complications (57.5%), difficulty walking or sitting (64.2%), bleeding from the genital tract (93.4%) were the commonly encountered physical consequences in a sexually abused child. Surprisingly, a mere 43.4% of mothers were aware that CSA would present as wounds/redness in the oral cavity and throat. A cross-sectional study conducted among mothers of primary school children in Tamil Nadu, India concluded that 76.9% of mothers had the awareness of unexplained genital injury was seen in child sexual abuse; 13.4% were aware of recurrent vulvovaginitis and 15.1% were aware of vaginal or penile discharge seen in sexually abused children [3]. The results of our study, while being comparable on awareness of unexplained genital injury (84%), a higher proportion of our study population were aware of vulvovaginitis (76.4%) and vaginal or penile discharge (83%). Only 9.7% of Indian mothers were aware of bed wetting and faecal soiling beyond the usual age as a possible result of CSA [3]. This physical consequence was also relatively poorly understood among Sri Lankan mothers (29.2%).
A meagre 12.9% of South Indian mother had awareness of anal complaints; 14.5% had awareness of pain on urination and 24.7% had awareness that sexually transmitted infections were associated with child sexual abuse [3]. Comparatively, our study revealed that 57.5% were aware of anal complications, 50.9% were aware of painful urination or defaecation and 83% of the current study population were aware that sexually transmitted diseases could be seen in children who were subjected to CSA.
A cross-sectional study conducted in Egypt revealed that the most dangerous complication anticipated following CSA was depression and it was experienced by more than half of the study population [9]. Similarly, 73.6% of our study population were aware that depression was an important psychological consequence of CSA. This is vital to be given considerable attention since childhood depression has many long-lasting consequences burdening not only the child but the healthcare system and society at large for years to come. Adolescent suicide is extremely concerning, and the impact of CSA should not be taken lightly since CSA is frequently under-reported.
The psychological consequences of CSA are arguably more consequential than physical consequences. The hidden trauma, which is not freely discussed or counselled in a deeply traditional country like Sri Lanka where such topics are associated with social stigma, should be properly handled by medical professionals along with the trusted relatives to ensure the child doesn’t suffer continuously. A literary work published on child and adolescent psychiatry documents that, children were affected adversely immediately or even later, the mental health of many was harmed in a variety of ways including depression, PTSD, anxiety, low self-esteem and self-harm, inappropriate sexual behaviour and conduct disorder. Harm was also found to extend into adulthood [10]. More specifically, particular emphasis was found to be warranted to address the two primary adjustment concerns known to affect sexually abused individuals: Type II or complex posttraumatic stress disorder (PTSD) and sexuality conditions [11].
A cross-sectional study conducted in Southern India revealed that 56.5% of mothers had the awareness regarding the problems at school; 83.9% had the awareness regarding acute traumatic response such as clingy behaviour and irritability and 54.8% had the awareness regarding sleep disturbances [3]. Contrastingly, our study revealed that 92.5% of mothers were aware of difficulty with schoolwork, 84% were aware of irritability or aggressiveness and 77.4% were aware of nightmares disturbing sleep as consequences of CSA. This reflects on the better understanding of Sri Lankan mothers regarding the various psychological consequences of CSA.
With regard to preventive strategies, a study conducted in Jordan revealed that 74% mothers believed CSA could be prevented by educating children [6]. Another study conducted among parents of pre-schoolers concluded that 59.1% discussed the dangers of child sexual abuse with their children.72.5% of the parents believed that all preschools and daycare centres should conduct child sexual abuse prevention programmes [12]. However, a higher percentage of mothers of our study educated their children, either constantly (71.4%) or occasionally (24.8%). Most of the mothers of children attending a primary school in China (60%) had already instructed their children to not allow strangers to touch their private organs and to say “No” if they felt threatened or uncomfortable [13]. An overwhelming majority of our study population (99%) stated they would actively participate in programs aimed at disseminating knowledge on preventing CSA.
The peak age of vulnerability has been found to be between 7 and 13 years which is an extremely impressionable age where young children undergo the already challenging and exploratory period of puberty. A systematic review concluded that cognitive-behavioral therapy (CBT) of the child and a nonoffending parent is the most effective treatment. This underlines the extremely important effect a trusting and loving parent has on preventing and recovering from CSA. Future studies should focus on implementing preventive programs and assessing their effectiveness.
Acknowledgements
Our sincere appreciation to all mothers who participated in the study and provided their valuable insight into a topic stigmatised in Sri Lanka. Our sincere thanks to all administrators who provided approval and support to make this study a success.
Conflicts of Interests
There are no conflicts of interest.
Abbreviations
CBT – Cognitive Behavioral Therapy
CSA – Child Sex Abuse
References
- Lifetime prevalence of child sexual abuse (%) [Internet]. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/lifetime-prevalence-of-childsexual-abuse-(-)
- Browne, A., & Finkelhor, D. (1986). Impact of child sexual abuse: a review of the research. Psychological bulletin, 99(1), 66.
- Shirley, S. A., & Kumar, S. S. (2020). Awareness and attitude of mothers of primary school children towards child sexual abuse in Tamil Nadu, India.
- AlRammah, A. A. A., Alqahtani, S. M., Babiker, A. G. E., Al-Saleh, S. S., Syed, W., Al-Mana, A. A. K., & Al-Shammari, H. H. (2018). Factors associated with perceptions of child sexual abuse and lack of parental knowledge: A community based cross-sectional study from the Eastern Province of Saudi Arabia. Annals of Saudi medicine, 38(6), 391-398.
- Sathiadas, M.G., Viswalingam, A. BMC Pediatrnam, K. Child abuse and neglect in the Jaffna district of Sri Lanka – a study on knowledge attitude practices and behavior of health care professionals. BMC Pediatr 18, 152 (2018). https://doi.org/10.1186/s12887-018-1138-3
- Alzoubi, F. A., Ali, R. A., Flah, I. H., & Alnatour, A. (2018, January). Mothers’ knowledge & perception about child sexual abuse in Jordan. Child Abuse & Neglect. Elsevier BV. http://doi.org/10.1016/j.chiabu.2017.06.006
- Browne, A., & Finkelhor, D. (1986). Impact of child sexual abuse: a review of the research. Psychological bulletin, 99(1), 66.
- Zhang, W., Chen, J., & Liu, F. (2015). Preventing Child Sexual Abuse Early: Preschool Teachers’ Knowledge, Attitudes, and Their Training Education in China. Sage Open, 5(1). https://doi.org/10.1177/2158244015571187
- Welson, N.N., Mohamed, Y.A. Awareness of different forms of child abuse among Beni Suef University students: descriptive survey. Egypt J Forensic Sci 9, 68 (2019). https://doi.org/10.1186/s41935-019-0174-y
- Glaser, D. (2015). Child sexual abuse. In Rutter’s Child and Adolescent Psychiatry (eds A. Thapar, D.S. Pine, J.F. Leckman, S. Scott, M.J. Snowling and E. Taylor). https://doi.org/10.1002/9781118381953.ch30
- Wolfe, V. V. (2006). Child Sexual Abuse. In E. J. Mash & R. A. Barkley (Eds.), Treatment of childhood disorders (3rd ed., pp. 647–727). The Guilford Press.
- Wurtele, S. K., Kvaternick, M., & Franklin, C. F. (1992). Sexual Abuse Prevention for Preschoolers: A Survey of Parents’ Behaviors, Attitudes, and Beliefs. Journal of Child Sexual Abuse, 1(1), 113–128. https://doi.org/10.1300/J070v01n01_08
- Jing Qi Chen, Da Guang Chen, Awareness of child sexual abuse prevention education among parents of Grade 3 elementary school pupils in Fuxin City, China, Health Education Research, Volume 20, Issue 5, October 2005, Pages 540–547, https://doi.org/10.1093/her/cyh012
- Finkelhor, D. (1994). Current Information on the Scope and Nature of Child Sexual Abuse. The Future of Children, 4(2), 31–53. https://doi.org/10.2307/1602522
- Putnam, F. W. (2003, March). Ten-Year Research Update Review: Child Sexual Abuse. Journal of the American Academy of Child & Adolescent Psychiatry. Elsevier BV. http://doi.org/10.1097/00004583-200303000-00